Each year, over 50,000 HIV care providers receive tailored HIV training from HRSA to better equip them to deliver HIV care to people with HIV with low incomes, according to a report from HRSA’s Ryan White HIV/AIDS Program (RWHAP).
Trainings reached a mix of nurses, doctors, social workers and others via group trainings and individual consultations. Training has evolved—in subtle ways—in terms of who gets training, in what format, and on what subject matter.
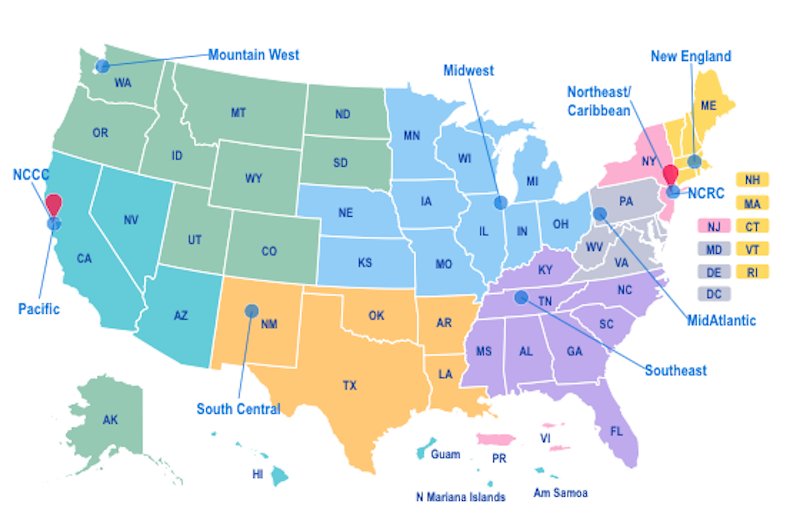
The AETC Program Annual Data Report, 2020 covers the time frame 2015-2020 and summarizes training as delivered by the eight regional AETC offices that are part of the broader HRSA AETC Program, which is the clinical training arm of the RWHAP. (See the sidebar for an overview of the AETC network.)
Shifts in Training Reflect Changes in HIV Care
The AETC report documents a notable shift in training formats and topics over the five-year time frame. For example, regional AETCs have reached greater numbers of multi-disciplinary staff who are non-prescribers.
Varied factors likely influenced this change.
- One is the evolving approach that includes adoption of evidence-based interventions that utilize the entire team in HIV care delivery, from clinicians to peers to social workers, in response to the multitude of client health and social needs. The AETC network has developed practice transformation resources to support these changes, while HRSA’s HIV/AIDS Bureau has supported identification of evidence-based interventions for replication by RWHAP agencies.
- Another possible influence in shifting trends is the increased number of online tools developed by the AETC network that allow staff to remotely access training and clinical support information. Examples include the National HIV Curriculum and the HIV/HCV Co-infection: An AETC National Curriculum.
Additional changes, in training audiences and topics covered, are outlined below.
Training Highlights
Training Topics
The most common topic in 2015-2016 was antiretroviral therapy or ART (49% of training events), followed by pre-exposure prophylaxis (PrEP). From 2017-2020, PrEP remained a leading topic with the addition of HIV prevention, while ART and other HIV primary care subjects remained leading subjects of interest. The increased interest in PrEP is likely attributable to the increase in PrEP options during that period including a generic brand of TDF/FTC and the FDA approval of TAF/FTC for PrEP use.
Formats
Trainings focused on “coaching organizational capacity building” became a newly reported training category in 2017 and was the most common training modality from 2017-2020. Examples include the Southeast AETC online Practice Transformation Curriculum. Formal presentations (i.e., didactic presentations, interactive in-person presentations, training workshops) remained somewhat constant in terms of proportions of total trainings. In-person events declined in early 2020 due to COVID-19 and distance-based learning became much more common.
Trainees
Nurses comprised the majority of training participants, followed by doctors and social workers. Approximately half of trainees are white, with slight increases (over the time frame 2015-2020) in Black/African American and Hispanic/Latino trainees. Nearly three out of four trainees provide direct clinical services, although more recent years have seen an increase in training participants who deliver HIV prevention counseling and testing services and prescribe PrEP. Additionally, across-the-board, one-fourth of trainees have less than one year experience delivering services to people with HIV.