The Alexis Project used social network recruiting and engagement, peer navigation, and contingency management to reach and engage transgender women of color with HIV who were not engaged in HIV care. With funding from a Ryan White HIV/AIDS Program (RWHAP) Part F Special Projects of National Significance (SPNS) initiative, the Friends Research Institute developed and implemented The Alexis Project from 2014 to 2016. Participation in the 18-month intervention improved linkage to care and viral suppression.
Transgender women in the United States, particularly women of color, are disproportionately impacted by HIV,1 due to multiple factors, including stigma, injection drug use, limited employment opportunities, and unstable housing.2 Structural and individual barriers to linking and retaining transgender women of color in HIV care may be overcome with models to encourage and motivate these women to engage in care. The Alexis Project used two distinctly different evidence-based behavioral interventions—peer health navigation and contingency management—to link and retain transgender women of color with HIV in HIV care.
A peer health navigator met with each client to develop a personalized treatment plan and directly link them to HIV primary health care and other needed physical, mental health, and/or psychosocial services. At the first session, the navigator conducted an assessment of the client's health history (including past HIV care), unmet service needs, and barriers to health care, and answered any questions about peer health navigation. Navigators also reminded clients about upcoming appointments and, if necessary, transported and accompanied them to all scheduled appointments. Clients were encouraged to have ongoing contact with their navigators during the 18-month intervention (usually two to three times per week during the first weeks of the relationship, which decreased after the first few months of care). Once this relationship was established with treatment plans being followed and barriers to auxiliary services reduced, navigators continued to support their clients to become more self-sufficient, building self-efficacy for sustained healthy behavior change.
Behavioral economics applies contingencies to motivate people toward health-promoting behavior change. This involves the provision of direct and immediate reinforcement for healthy or health-promoting behaviors. The principle of contingencies, i.e., making the reward contingent upon the operant behavior change, is what distinguishes this from just providing a traditional incentive.3
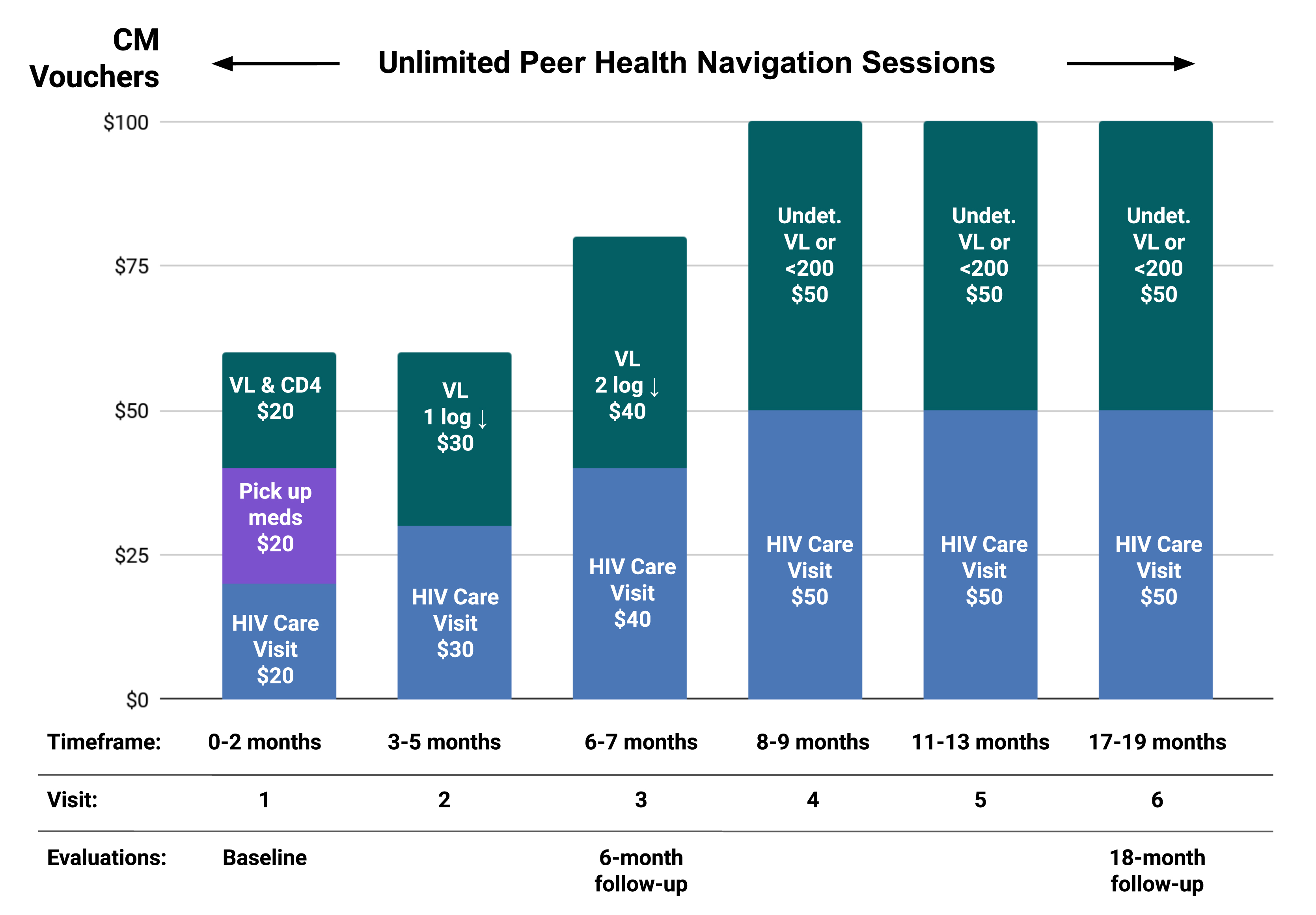
Alexis Project staff used contingency management to improve health outcomes by specifically focusing on HIV primary care appointments and HIV milestones (e.g., undetectable viral load) for positive reinforcement. People received points that could be exchanged for goods and services when attending HIV visits, picking up medications, and reaching or sustaining viral suppression. Each point was equivalent to $1 and was used toward goods or services of the client’s choosing. These included gift cards to grocery or department stores, clothing, wigs and make-up, electrolysis and other skin care services, other gender-promoting services, and computer equipment.
Alexis Project staff used a social networking methodology, grounded in respondent-driven sampling (RDS) for recruitment. Staff provided coupons that incentivized participants from “hidden populations” to recruit peers to enroll into the intervention. RDS is maximally preferable when the population in question is not only hidden, but relatively closed (i.e., social networks tend to contain members from the same group exclusively), such as transgender communities.4
From February 2014 through August 2016, 139 transgender women of color enrolled in The Alexis Project. Participants self-identified their race/ethnicity as African American/Black (41.0%), Hispanic/Latina (31.7%), multi/other (21.6%), and Native American (5.8%). At baseline, 26% had never been in HIV care and, among those who had previously been in HIV care, 41.9% percent were disconnected. Furthermore, at baseline, 48.2% were in need of an antiretroviral therapy (ART) prescription, and 51.1% had one but were non-adherent. On average, Alexis Project participants attended 6.6 peer health navigation sessions. Participants also made 648 milestones, earning a total of $19,960 in points (for an average of $143.60). At intervention completion, the majority of the participating clients were linked to care and just under half had reached and/or maintained viral suppression.
| Category | Information |
|---|---|
| Evaluation data |
|
| Measures |
|
| Results | After 18 months in the intervention:
|
Source: Enhancing Linkages to and Retention in HIV Primary Care for Transgender Women of Color: The Alexis Project. Intervention Manual. 2018.
Peer health navigator training. Transgender women of color with HIV were integral to staffing as peer health navigators and received ongoing training and support throughout the project. The initial training included sessions on creating and setting boundaries, writing progress notes, maintaining confidentiality, developing active listening skills, understanding countertransference, and self-care. Additionally, a PhD-level clinician provided semi-monthly supervision to the navigators, while an HIV infectious disease physician served as the medical advisor, and delivered an annual training on HIV care and the interpretation of medical records to the navigators. The medical advisor also provided ongoing individualized interpretation of medical records, reviewed hormone treatment profiles and ART choices as needed, and guided navigators on how to coach participants to reach and sustain their HIV milestones.
Input from community. Friends Community Center, a community research center affiliated with the Friends Research Institute, has a long-standing transgender community advisory board that provided input on design, implementation, and recruitment for the intervention, along with feedback on improving the project and overcoming barriers. Board members also provided feedback on enrollment, implementation, monitoring activities, and approaches to outreach.
Outreach and recruitment. Outreach and recruitment strategies included: 1) respondent-driven sampling, a community-wide social network recruitment and engagement methodology; 2) venue- and street-based outreach in locations such as restaurants and bars where transgender women tended to congregate; 3) dissemination of a postcard-sized flyer and a business card-sized flyer that fit in a person’s wallet or pocket; 4) in-reach through other programs at Friends Community Center; 5) in-services at local agencies that provided services to transgender women; and 6) community partners, namely two HIV medical care clinics that referred potential participants to the project.
- While originally funded through the RWHAP Part F SPNS initiative, some services, such as intensive case management and peer navigation, were covered through other RWHAP Parts.
- The maximum dollar amount a client could receive was $500 for reaching all HIV health-promoting goals, so the total dollar amount allocated for incentives depended on the number of participants as well as how many goals they achieved.
- Peer health navigators provided clients with 18 months of unlimited sessions to address any barriers that impeded their ability to be linked and retained in care. Navigators helped clients secure housing, access to substance use treatment facilities, clothes and hygiene products, and food, and addressed a number of other barriers impacting their quality of life. With this comprehensive support, most clients wanted to remain in The Alexis Project, as their most basic and critical needs were being met.
- Retention was boosted through the rapport built between clients and navigators, true peers—transgender women of color with HIV. Clients felt safe to discuss barriers to linkage and retention in care, as well as issues related to medication adherence.
- Navigators required ongoing training, guidance, and support to adhere to the personal and professional boundaries needed to work effectively. Given that navigators were peers, they had experienced many of the same issues that the participants were experiencing. The emotional weight of working closely with participants and not being able to solve every issue proved to be trying; the decision was made to provide navigators with a clinical supervisor who was available to discuss specific client situations as well as the inherent difficulties of working with transgender women of color with HIV. Through this supervision and training, peer health navigators learned to set appropriate boundaries and how to be of assistance to clients without taking on the weight of their worries.
- CDC. HIV Infection, Risk, Prevention, and Testing Behaviors Among Transgender Women—National HIV Behavioral Surveillance, 7 U.S. Cities, 2019–2020. HIV Surveillance Special Report 27. 2021.
- Song W, Mulatu MS, Rao S, Wang G, Kudon HZ, O’Connor K. HIV partner service delivery among transgender women—United States, 2013–2017. MMWR Morb Mortal Wkly Rep. 2020;69(2):35–39. doi:10.15585/mmwr.mm6902a3
- De Walque D, Dow WH, Nathan R, Abdul R, Abilahi F, Gong E, et al. Incentivising safe sex: a randomized trial of conditional cash transfers for HIV and sexually transmitted infection prevention in rural Tanzania. BMJ open. 2012;2(1). doi:10.1136/bmjopen-2011-000747
- Boyce S, Barrington C, Bolaños H, Galindo Arandi C, Paz-Bailey G. (2011). Facilitating access to sexual health services for men who have sex with men and male-to-female transgender persons in Guatemala City. Culture, Health, & Sexuality, 14, 313-327. doi: 10.1080/13691058.2011.639393
