Southeast Mississippi Rural Health Initiative, Inc. (SeMRHI), a network of community health centers serving Southern Mississippi, uses data-driven quality improvement techniques to identify youth who are not virally suppressed or have missed appointments. Medical case managers use a client checklist to identify and address barriers to antiretroviral therapy (ART) and medical care adherence. They also use a health literacy visual illustration tool to help youth understand the effects of ART on viral suppression. The intervention strategy was successful in improving viral suppression rates for youth.
MS
SeMRHI conducted a quality improvement project in 2017 as part of the end+disparities ECHO Collaborative through the Ryan White HIV/AIDS Program (RWHAP) Center for Quality Improvement & Innovation (CQII) that revealed youth with HIV had the lowest viral suppression and retention rates of all their clients with HIV. These youth had very high viral loads, with only 55% reaching viral suppression. Also, many who were unsuppressed were lost to care. Identified barriers to care included untreated behavioral health issues, unstable housing, multiple missed appointments due to work and/or school schedules, and stigma. Another factor was low health literacy in understanding HIV and the impact of medication adherence on viral load.
SeMRHI uses a data-driven quality improvement approach to identify and reach out to youth who are not virally suppressed or who have missed appointments.
SeMRHI medical case managers (registered nurses and social workers) use a patient checklist to identify barriers to engagement in care, ART adherence, and viral suppression, which they administer with clients either via phone or during client visits. The case managers refer youth to appropriate services including behavioral health, housing, transportation, food pantry, and community resources.
The medical case managers also use health literacy aids, including a bead adherence illustration tool. This tool uses beads to explain visually the effect of ART on viral suppression, in a manner that meets the health literacy needs and developmental level of youth.
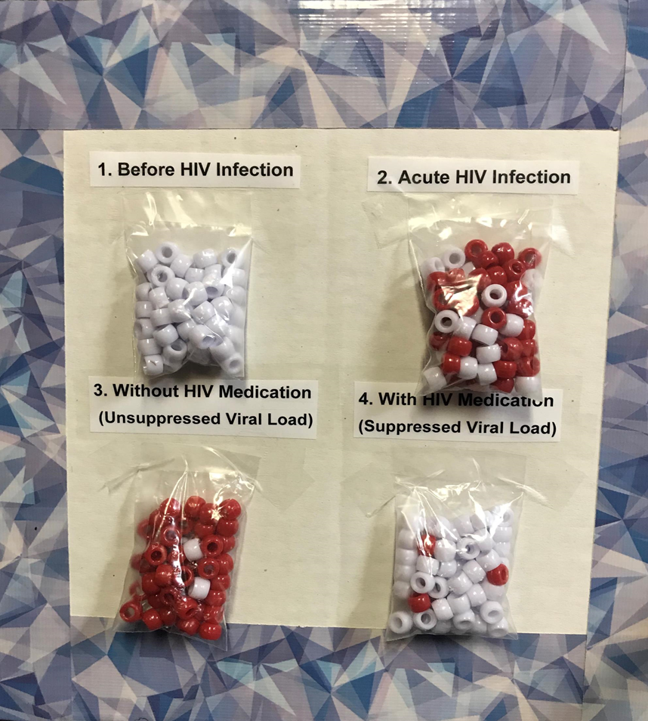
Bead Adherence Illustration Tool
The social worker (LCSW) provides face-to-face or telebehavioral health visits to manage mental health and substance use issues affecting the health of youth.
An Adherence Case Manager (LPN) immediately follows up via phone call with youth who missed their medical appointments.
The intervention strategy was successful in improving viral suppression rates for youth, defined as ages 13 through 24.
| Category | Information |
|---|---|
| Evaluation data | Monthly data generated from performance measures in CAREWare. |
| Measures | Viral suppression. |
| Results |
Over a 12-month period from July 2018 to June 2019, viral suppression rates for youth increased from 58% to 78%. The viral suppression rates for youth continue to be sustained at or above 75%. |
Source: Achieving Viral Load Suppression in Youth Living with HIV in South Mississippi. National Ryan White Conference on HIV Care & Treatment 2020 presentation.
"Most 16–18-year-olds are still in high school or in college, or they may have dropped out of high school. They can tell you everything about Snapchat and Instagram, but they do not know what viral load means. Being able to break down such complicated words and terminology into a visual that they can understand is an important factor to learning. Our goal is to meet the patient where they are. We can't use those big fancy terms that they may not understand.”
- SeMHRI implemented a data-driven, quality improvement approach to identify youth aged 13-24 with low viral suppression rates or with missed appointments.
- To improve clients’ understanding of the importance of ART adherence, SeMHRI identified health literacy tools, including the bead illustration tool.
- SeMHRI adapted the patient checklist featured in the end + disparities ECHO collaborative, for use with its own clients.
- This strategy is now fully integrated for youth clients in the SeMHRI network. Due to its success, SeMHRI will expand the intervention to clients of all ages who are not virally suppressed.
- SeMHRI health centers continuously review and discuss with staff the intervention strategy and its alignment with the HIV care continuum.
- SeMHRI has prioritized and formalized the clinical quality improvement approach and advocates for adequate staff to employ this component.
- Despite these strategies, some youth do not reach viral suppression due to factors including stigma, behavioral health status, denial of diagnosis, maturity level, cognitive function, and other social determinants of health factors.
- It is important to continue to address ongoing barriers to care, such as missed appointments; lack of adherence to ART; failure to complete ADAP recertification; and behavioral health indicators.
- Meet the clients where they are by accommodating their cognitive learning needs and behavioral health issues when providing care.
- Advocate for people over policy; it is not a one-size fits all.
“The client is the best resource. I would personally conduct phone calls during missed appointments to assess barriers that contribute to their missed doctor's appointments. From their responses, we develop a checklist. From that checklist, we identified certain goals to help decrease those barriers.”

