“The door to darkness had been opened, and all the taboos were out there—sex, death, homosexuality, drug use. Things that people had never heard discussed openly before.”
– Cliff Morrison, who established Ward 5B/5A at San Francisco General Hospital in the early days of the epidemic

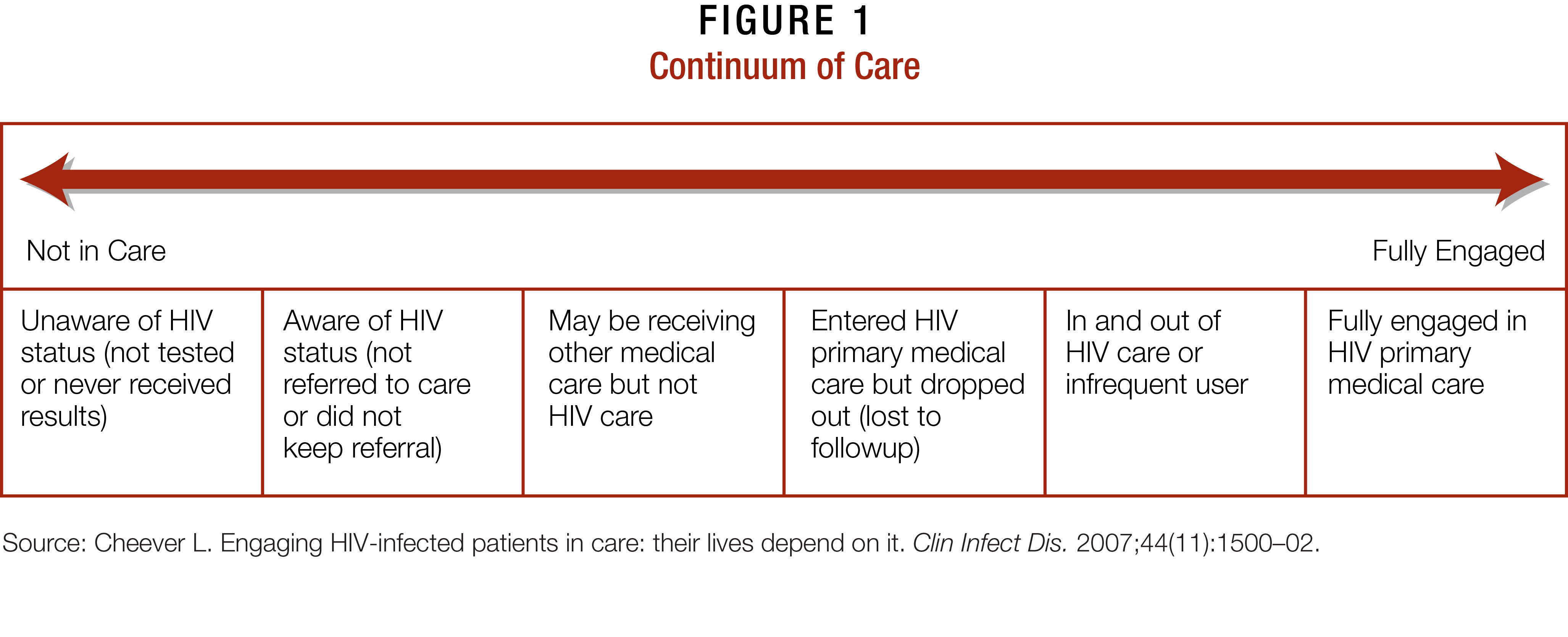
HRSA conceptualizes engagement in HIV care as a spectrum, as opposed to a singular event, that begins with PLWHA learning their serostatus and ends with their full engagement and retention in HIV primary care (see Figure 1). Numerous factors prevent PLWHA from moving smoothly from one end of the spectrum to the other. For instance, a large number of PLWHA have never been screened for HIV, and others have been tested but never learned their results. Still other PLWHA know their status but have not been referred to care; have never followed up on their referral; are in care, but not for HIV; or have fallen out of HIV care or seek it sporadically due to a variety of reasons. The location of PLWHA along the spectrum is not static. Rather, they move up and down the continuum in response to unmet needs, such as those related to food insecurity and shelter instability (FISI), poverty, substance use disorders (SUDs), mental illness, and other psychosocial and economic determinants.7 PLWHA with limited educational attainment and histories of incarceration also have difficulty obtaining and maintaining employment and health insurance, which can further delay them in accessing care. It is not uncommon for PLWHA to ignore their health needs until they require emergency room assistance. Seeking assistance from an HIV primary care provider often marks their first ongoing experience with the health-care system.8
You hear stories that people are still very much ashamed to have HIV due to religious beliefs and cultural stigma. People view the disease with a lot of disdain and blame those who are living with it. There are certainly huge barriers that will exist [to testing and care].
-Michael K. Evanson, senior policy analyst in the Division of Science and Policy at HRSA, HAB
The need for PLWHA to seek HIV treatment as soon as possible in their infection cannot be overstated. Research has shown consistently that PLWHA who are engaged in a holistic spectrum of care, such as that offered by Ryan White HIV/AIDS Program providers, are more motivated to keep appointments; initiate and adhere to antiretroviral therapy (ART); regularly get required lab work done; and participate in support services, such as mental health, SUD and alcohol counseling, and dental care. They, along with their families, also are more likely to leverage ancillary/wraparound services facilitated by Program providers, such as transportation, food and clothing banks, and health education classes.9-13
Early HIV intervention and treatment improve PLWHA health outcomes. Costs of early interventions are also significantly cheaper—sometimes by more than 50 percent—than those associated with late HIV infection and end-of-life care.14,15 Moreover, PLWHA in care are less likely to engage in high-risk behaviors, such as unprotected sex and injection drug use (IDU), which decreases transmission of HIV and comorbidities such as hepatitis. These PLWHA are also more likely to take their ART consistently, mitigating their chances of becoming resistant to HIV medications and progressing to AIDS.16-19
Despite the potential for these positive health outcomes, a large number of PLWHA do not engage in care, or fall out of care shortly after starting it. For instance, approximately 35 to 45 percent of PLWHA are tested for HIV later in their infections, as indicated by their diagnosis with both HIV and AIDS and/or progression to AIDS within a year of their HIV diagnosis. These late testers most likely have had HIV for longer than 5 years, during which their immune system as well as potential success in ART have been significantly undermined.
Considering the health potential of HIV services, many in the health-care community continue to question why people wait so long to get tested and engage in HIV care. The reasons, however, are reflected in the interplay of psychosocial, culturally, and community-based determinants that steer the lives of many people who are members of populations heavily impacted by HIV.20,21 A more in-depth examination of communities disproportionately impacted by the disease—African-Americans, Hispanics/Latinos, Asians, Native Hawaiians/Pacific Islanders (NH/PIs), and American Indians/Alaska Natives (AI/ANs)—and the barriers and stigma they face provides a greater understanding of the complexities around engaging hard-to-reach PLWHA into care.
THE IMPORTANCE OF HIV/AIDS CARE
Retaining patients in care results in better health outcomes.
Attending all medical appointments during the first year of HIV double survival rates for years afterwards regardless of baseline CD4 cell count or use of ART.
Giordano T, Harman C, Glifford A, et al. Predictors of retention in care among a national cohort of US veterans. HIV Clin Trials. 2009;10 299-305
HIV Stigma — More Than 30 Years in the Making
Many PLWHA do not seek testing or care because of the stigma associated with the disease. Soon after HIV/ AIDS was first described in the CDC’s Morbidity and Mortality Weekly Report (MMWR) in 1981,22 the disease became synonymous with White gay men. Sources for the first New York Times article about AIDS attributed the illness to “homosexual men [having] multiple and frequent sexual encounters with different partners, as many as 10 sexual encounters each night up to four times a week.23 In the same piece, James Curran, a medical doctor, said “nonhomosexuals” had no reason to worry since “no cases have been reported to date outside the homosexual community.23
Early names for HIV/AIDS infection, such as gay cancer, gay-related immunodeficiency or GRID, gay compromise disorder, and community-acquired immune dysfunction,24-26 further stigmatized the disease, as did the declaration of official risk groups. Known as the “4H club,” these groups included Haitians, homosexuals, heroin users, and hemophiliacs. All but hemophiliacs were vilified in the press, although children infected by HIV-contaminated blood product, including Ryan White and the Ray brothers of Florida, were not spared by their local communities. Many HIV-positive children and their families left their homes in the wake of death threats and violence.27,28
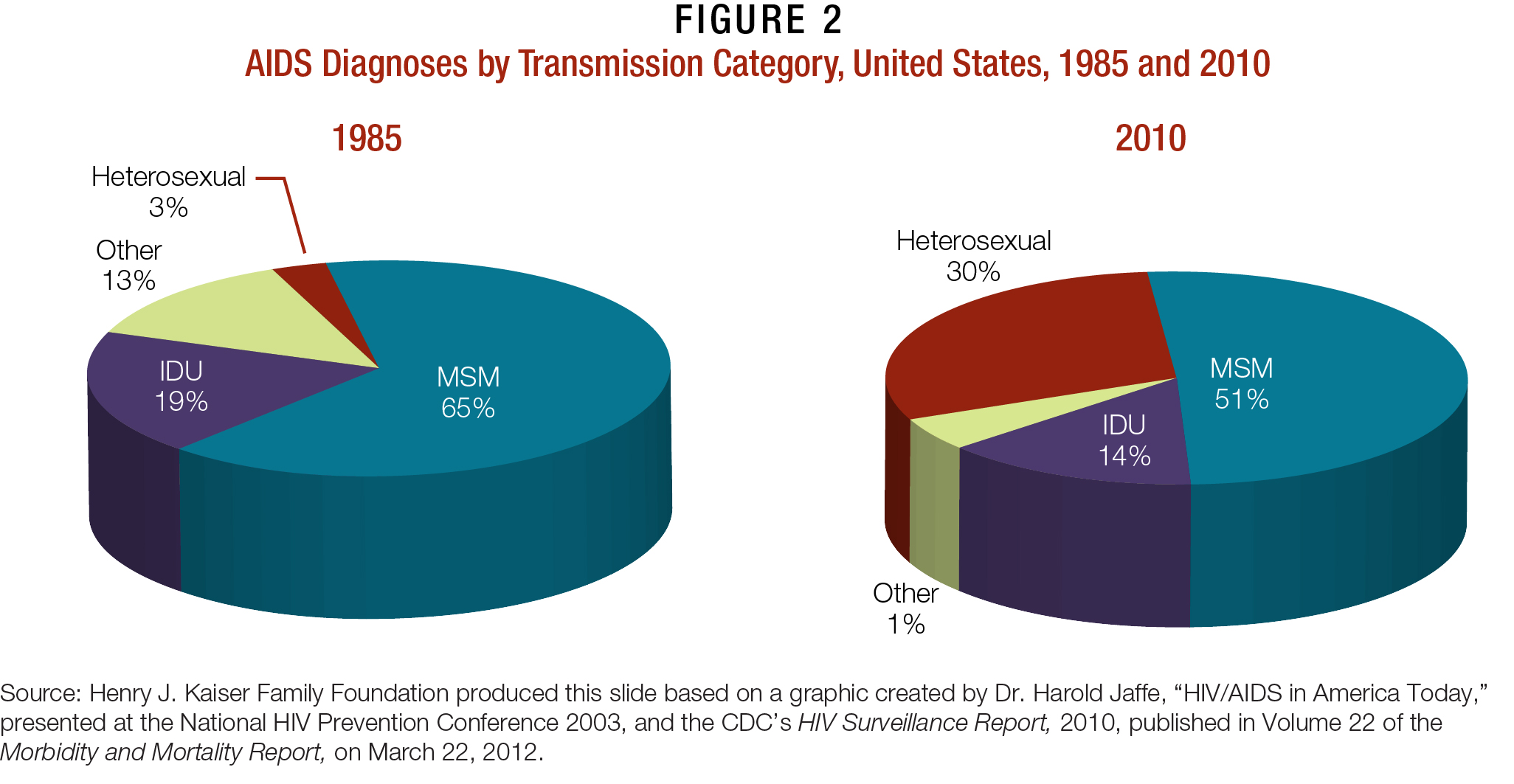
These misguided notions continue to persist, even though the disease was renamed in 1982 and, soon after, diagnosed in women, children, adolescents, and heterosexual men.29-31 Caribbean and African immigrants, and men who have sex with men (MSM) in particular, continue to be blamed by many for introducing HIV/AIDS to the U.S. population, though nearly one-third of estimated AIDS diagnoses cases in 2010 were attributed to heterosexual contact, compared to 3 percent in 1985.29,32
Communities Heavily Impacted by HIV
To this day, HIV is often perceived as a “gay, White man’s disease,” leading many people, including members of underserved and marginalized populations—such as urban-based MSM of color—to believe they are not personally at risk. This may be the case even if they know others in their community living with HIV/AIDS. This is particularly true among youth, who can feel invincible and, if infected with HIV, are not far enough along in their disease to feel ill.33-36 The disease has changed in terms of its geographic location. What started as primarily an urban disease quickly moved to rural pockets, particularly in the South.37,38
Ethnic and racial minorities bear the greatest HIV burden within the United States. They account for nearly 70 percent of the approximately 50,000 new HIV cases diagnosed every year; well over one-half of all PLWHA nationwide;39 and the majority of all HIV/AIDS deaths since the start of the epidemic.40 While African-Americans and Hispanics/Latinos bear the greatest burden of HIV in the country, the disease has also disproportionately impacted Asians, NH/PIs, and AI/ANs. It also continues to devastate populations that cut across these communities, including gay men/MSM and IDUs.
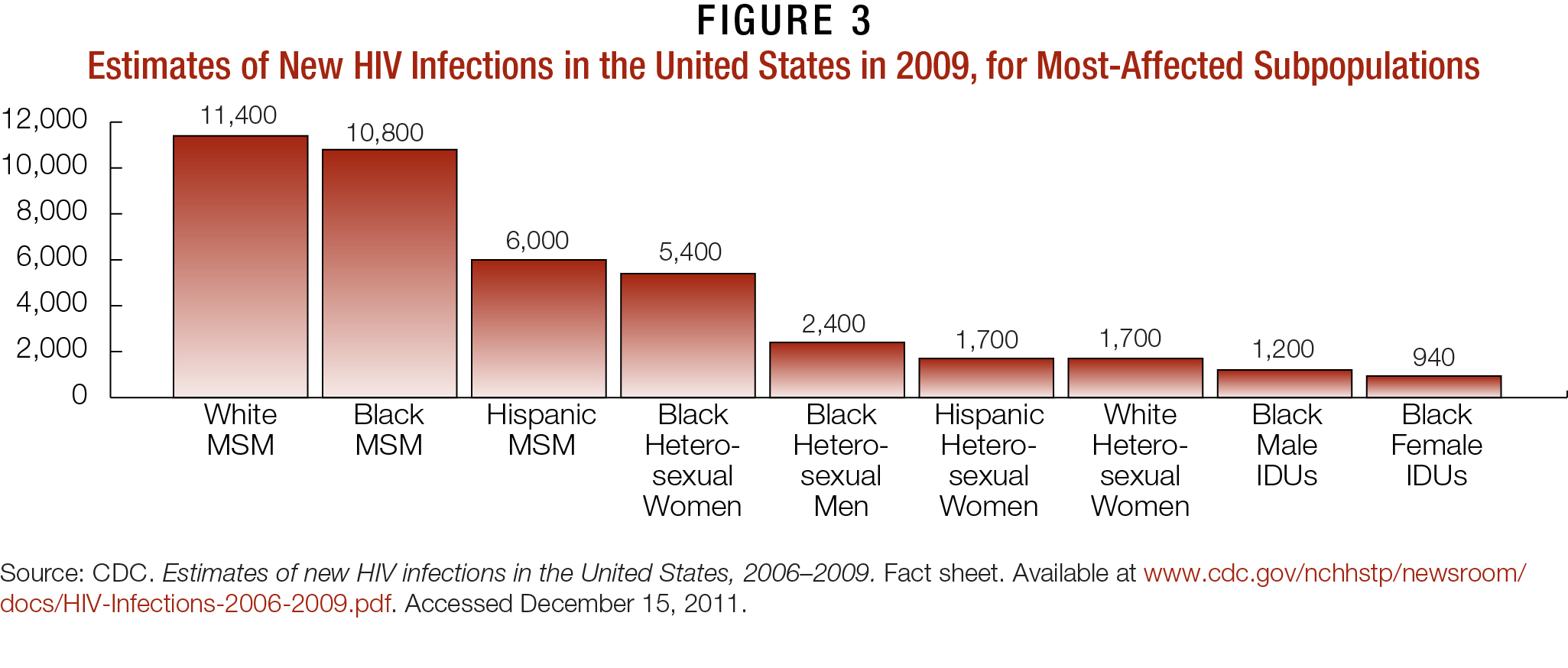
Perhaps most distressing is that PLWHA in these communities tend to learn their status later and progress to AIDS sooner than their White counterparts. In fact, the CDC reported in 2009 that 31 percent of Blacks, 37 percent of Hispanics/Latinos, 29 percent of AI/ANs, and 34 percent of Asians received an AIDS diagnosis within 12 months of being diagnosed with HIV.32 Engaging PLWHA in these communities into care and ART is essential to ending the AIDS epidemic.
HIV Prevention Trial Network (HPTN) 052 demonstrated that ART reduced HIV transmission to uninfected partners by 96 percent.41 ART also has been linked to decreasing rates of new HIV infection diagnoses and overall community viral load in areas with high concentrations of PLWHA and persons at high risk for HIV, such as MSM and IDUs.41,42 In addition, ART is linked to reducing HIV-related morbidity and mortality and perinatal HIV transmission,43,44 and is shown to decrease inflammation and immune activation. The latter tends to occur more often among PLWHA than their HIV-negative counterparts, and may be linked to cardiovascular and other organ damage.41
Please refer to the appendices for specific overviews concerning the impact of HIV/AIDS within African- American/Black, Latino/Hispanic, NH/PI, and AI/AN communities, as well as among women, incarcerated PLWHA, MSM and young MSM.
SEEKING A MODEL OF CARE THAT SPECIFICALLY ADDRESSES PLWHA LIVING WITH SUBSTANCE USE DISORDERS?
Clinics and other stakeholders interested in integrating SUD treatment into HIV primary care may be interested in the IHIP training manual, curriculum, and online trainings, Integration of Buprenorphine into HIV Primary Care Settings.
These materials provide HIV primary care providers information and training materials necessary to integrate medication-assisted treatment (MAT) with buprenorphine into HIV primary care. They provide a detailed overview of buprenorphine within clinical settings, from the legal requirements for implementation to step-by-step procedures for prescribing and administering buprenorphine.