The goal of the CQII Quality Award Program is to celebrate the success of Ryan White HIV/AIDS Program (RWHAP) recipients, subrecipients, and individuals nationally, increase the visibility of quality champions, and provide real world examples of quality improvement (QI) that other programs could aspire to achieve.
The 2024 CQII Quality Awards include the following award categories:
- Measurable Improvements in HIV Care
- Involvement of People with HIV in Quality Improvement
- Leadership in Quality Improvement
For details regarding each award category and selection criteria, please review the 2024 CQII Quality Award Categories and Selection Criteria.
Submit Nominations
We invite you to submit nominations by Friday, April 12, 2024, using the following steps:
- Download and review the 2024 CQII Quality Award Categories and Selection Criteria document on the TargetHIV.org website to better understand the award categories and selection criteria.
- Submit your application, along with the Supporting Documentation.
A panel of Health Resources and Services Administration (HRSA) HIV/AIDS Bureau (HAB) and CQII staff will review each application utilizing the respective review criteria. The improvement stories and pictures of the 2024 CQII Quality Awards winners will be shared via CQII announcements, on the CQII landing page on the HRSA HAB TargetHIV.org website, and possibly on future national CQII technical assistance calls.
If you have any questions, please contact Andrea Mayer at 212-417-4730 or via email.
We look forward to receiving your nominations and reading about your improvement successes.
2023 Quality Awards
Evergreen Health Services, Buffalo, NY

From left to right: Collin Ranney, Patient Experience Manager, Jillian Fanning, Quality Manager, Andrew Kiener, Associate Vice President of Quality.
We congratulate Evergreen Health Services for their outstanding work in quality improvement (QI) and we are honored to present them with CQII’s 2023 Award for Patient Involvement in Quality Improvement.
Evergreen Health, formerly known as AIDS Community Services, was founded in 1983 to address the AIDS crisis in Western New York. As breakthroughs in medical treatment were made for HIV and other sexually transmitted infections, the organization expanded its range of services beyond HIV care to meet the needs of the local community. Through this expansion, the Evergreen Health Quality/Patient Experience Team was formed, evolving from one individual handling client feedback and satisfaction into a team of nine dedicated to meaningful client satisfaction, participation, feedback, and navigation. The team is proactive in introducing innovative approaches, utilizing both qualitative and quantitative standards and metrics to assess and enhance the quality of services. Collin Ranney, Patient Experience Manager, cites the culture among the staff as one of the key ingredients in their success: “Staff engagement is an important element to the enhancement of patient experience. I think with good staff comes good patient experience.”
COVID-19 and New Feedback Channels
The COVID-19 public health emergency created obstacles for Evergreen Health that affected their ability to gather written and in-person client feedback and led to the suspension of meetings for their longstanding Partners Group, the organization's client advisory board (CAB). Andrew Kiener, Associate Vice President of Quality, noted that “we didn’t have the numbers we had…or the groups that we could hold, or things that we could get feedback from. It became especially apparent then that the agency needed to concentrate more efforts on patient experience.”
Evergreen Health adopted Patient Pulse, a direct-to-patient survey platform to gather feedback.
In response to these challenges, Evergreen Health introduced a direct-to-patient survey platform called Patient Pulse. After a patient's appointment, personalized surveys are sent via text or email, enabling patients to share feedback on patient experience, satisfaction, and departmental clinical quality. Surveys provide an opportunity for Evergreen Health Services to receive responses to specific questions as well as for patients to share anything they would like in free text responses. A dashboard consolidates each survey response and survey data is used to improve staff engagement and patient support.
To enhance feedback collection, comment card boxes were also installed at six Evergreen Health locations. The boxes include QR codes and website integration, and their signage and promotion have been improved. “It’s been trial and error with our comment cards because they started off so small and now, we’re seeing more feedback on those because of the different ways we’re implementing them throughout the agency,” said Jillian Fanning, Quality Manager. Concurrently, a workgroup was formed to revitalize the Partners Group. They secured a budget, developed applications, and conducted a recruitment promotional campaign. By March 2023, the Partners Group was fully revitalized and currently holds monthly meetings, and many of these patients serve as mentors in recruitment and training of less experienced patients who want to get involved or have their voices heard. A survey to assess the need for a Caregiver Advisory Board is also in development, seeking to bring together parents, legal guardians, and professional health care caregivers.
From July through November 2022, Evergreen Health conducted a comprehensive 27-question Patient Experience Survey. This survey was designed to evaluate the experiences of individual patients, irrespective of the location site, clinical or non-clinical setting, or type of service received. Notably, specific Health Equity questions were included in the survey to gauge the fairness and access to opportunities that patients need to achieve their optimum level of health.
All these efforts resulted in the collection of 1,783 responses regarding individual patient experiences in 2022, a 138% improvement from 2021 and well exceeding the organizational goal of 65%. “It’s taking an idea and growing not only with the times but with the changes in the environment or with the patients that we serve because they change too,” said Andrew. The data they collect is also vital to their grant reporting processes and allows them to accurately report on patient experience initiatives to their funders.
Patient experience not only increases retention and improves health outcomes, but it also lets the community know that people with lived experience will be welcomed and heard. Andrew Kiener, Associate Vice President of Quality
Evergreen Health has long prioritized patient experience at every level of care because they understand that patient experience not only increases retention and improves health outcomes, but it also lets the community know that people with lived experience will be welcomed and heard. Andrew emphasized “Every voice is important. Whatever your economic background is, your color, your sexual interest, or anything else, none of that matters to us. If you’re a patient here at Evergreen, your voice is important.”
Evergreen Health Services demonstrated their commitment to engaging patients and gathering the input of community voices to improve the quality of care. We are honored to present them with CQII’s 2023 Award for Patient Involvement in Quality Improvement.
Contact Information
Collin Ranney
Patient Experience Manager
[email protected]
716-847-2441
Evergreen Health Services
DAP Health, Palm Springs, CA

From left to right: C.J. Tobe, Chief of Community Health, Jessica Ward, Early Intervention Supervisor, Trent Broadus, NP, Clinical Supervisor of Sexual Wellness, Denise Velasquez, Community Health Data Management Specialist, Mark DeJarnett, RN, Nursing Manager of Sexual Wellness.
We congratulate Desert AIDS Project, d/b/a DAP Health, for their outstanding work in quality improvement (QI) and we are honored to present them with CQII’s 2023 Award for Leadership in Quality Improvement.
The Desert AIDS Project was founded by a community of grassroots volunteers in Palm Springs, California in response to the AIDS epidemic in 1984 and achieved federally qualified health center designation in 2015. They have taken the lessons learned through the AIDS crisis to offer medical care and wraparound services addressing social determinants of health for the broader community regardless of HIV status. This led to the brand evolution to DAP Health in 2021.
Quality Improvement in Rapid ART
In 2019, DAP Health was awarded a Health Resources and Services Administration’s Special Projects of National Significance grant for rapid start antiretroviral therapy (ART) initiation. Today the Rapid Start ART Program consists of outreach, testing, community partnerships, a robust linkage to care program called Early Intervention Services (EIS), and two free sexual wellness clinics. The program provides ART to newly diagnosed, new to care, and out of care people with HIV in the sexual wellness clinics located in Palm Springs and Indio, California. The EIS program also offers incentives for clients who may need food, transportation to and from appointments, Tracfones for telehealth visits with their care team, and access to other community resources. The team saw measurable improvements in patient outcomes. DAP Health’s process improvements are impressive because of several successful Plan-Do-Study-Act (PDSA) cycles. These include a reduction in average wait times for new to care and out of care people with HIV to start ART from 59 days to less than 5 days. Currently, all rapid start patients at DAP Health obtain ART within three days.
The Role of Teamwork
When asked about their secret to success, C.J. Tobe, Chief of Community Health, shared that it’s always been teamwork. He expressed that “everyone gets a voice in what they want their role to be,” and how to meet the needs of the communities they serve. For example, the community health programs, sexual wellness clinics, and the mobile clinic staffs co-create the performance measures they want to monitor and conduct PDSAs for quality improvement.
“Everyone gets a voice in what they want their role to be.” C.J. Tobe, Chief of Community Health
To facilitate this kind of teamwork across the organization, DAP Health adjusted their business plan in 2019 and combined the community health department with their sexual wellness clinics. Doing so streamlined the process of testing, outreach, education, linkage to care, clinical care, rapid start, STI testing and treatment, and Pre-Exposure Prophylaxis (PrEP) and Post Exposure Prophylaxis (PEP). After these changes, DAP Health was able to increase staffing, make services free of cost, prospect additional grant funding opportunities, and quadruple the number of patients seen. Leadership continues to foster and maintain strong relationships throughout the organization, while uniting around the sentiment that they are all there to serve the patient, regardless of what door they enter.
Facing Challenges
While having achieved significant success in QI, DAP Health has also faced some challenges. The team talked about the common struggle of establishing staff buy-in with QI work. Staff can be overwhelmed and fear that QI leads to extra work but C.J. shared that they “invite everybody that’s going to be impacted by that change to have a voice in what change is going to look like.” Among their words of wisdom, creating a structure and standardization as a team was one of DAP Health’s suggestions for people starting out in QI, as this helped immensely with their staff’s ability to embrace change. C.J. defined leadership as an understanding that the organizational mission cannot be achieved by one, but by a team. He shared with us the importance of stepping back from the spotlight and empowering staff, community partners, and people with lived experience to find and share their own ideas for process changes and quality improvement. Jessica Ward, Early Intervention Supervisor, added how crucial having a diverse team representative of your client community is to provide high-quality holistic care.
The team at DAP Health exemplifies great leadership and commitment to quality and we are honored to present them with CQII’s 2023 Award for Leadership in Quality Improvement.

Left to right: Community artists Evelyn Sofia Riveria and Cece Cruz pictured with the Mujeres Murals at DAP Health Indio Clinic, located in Indio, CA.
Contact Information
C.J. Tobe, MA, Chief of Community Health
[email protected]
760-969-5742
DAP Health
Nassau University Medical Center, Long Island, NY

From left to right: Row 1: Concetta Bjelland, ID Division Secretary; Martine Michel Toure, MA, Administrator, Client & Medical Case Mgmt. Services; Shadab Ahmed, MD, Chief, Division of Infectious Disease; Grace Ting, Chief Medical Officer, NUMC; Tabassum Yasmin, MD, Director of HIV Services - Row 2: Hope Sender, HIV Program Coordinator; Barbara Galland LPN; Geraldine Jean-Baptiste, MCM; Michelle Campbell, MCM - Row 3: Olga Pimentel, MA, RPSSI; Fitsum Getachew, Data Manager; Russel Cascabel, RN - Row 4: Franklin Moquete MCM; Hamid Pahlevan, MD, QI/ Grant Manager, AHE-RAP Supervisor; Lemar Nadi, MD, Infectious Diseases Attending; Daniel Velazquez, MCM (MCM: Medical Case Manager, RPSSI: Regional Prevention & Support Services Initiative, AHE-RAP).
We congratulate Nassau University Medical Center (NUMC) for their outstanding work in quality improvement (QI) and we are honored to present them with CQII’s 2023 Award for Leadership in Quality Improvement.
The NUMC has a longstanding history serving diverse communities in Long Island, New York as the area’s first New York State Designated AIDS Center. What began as a 200-bed general hospital in 1935 is now a 1,200-bed healthcare system, including the 450-bed A. Holly Paterson Nursing home. NUMC is moving toward a new model of care that emphasizes excellent hospital and ambulatory services, primary care in the community, shared responsibility for wellness, and integrated delivery of specialty services. With community impact that spans close to a century, the NUMC leadership has demonstrated excellence in continually adapting to the everchanging needs of the diverse communities they serve.
Dr. Shadab Ahmed, Chief, Division of Infectious Diseases, Department of Medicine, reflected on her long career in HIV medicine since 1989 and how the years before antiretroviral therapy were filled with immense loss. “The satisfying thing is that we have come a long way, and there are people–a huge number of our patients–who are undetectable, who are living a normal life, have gone back to colleges, have gone back to work, have gone back to relationships.”
The Crucial Role of Data in QI
NUMC's Center for Positive Health (CPH) has been exemplary in promoting a culture of QI through their active participation in quality management committees, workgroups, and trainings offered by New York State Department of Health AIDS Institute. Throughout the years, CPH has strived to provide their clients with the best HIV care by continually implementing QI efforts across all programming. CPH’s senior leadership encourages all staff to participate in QI. Dr. Hamid Pahlevan, Grant Supervisor/Counselor, discussed how QI efforts have dramatically transformed since 2014 when the clinic wanted to improve viral suppression rates in the patient population. Dr. Pahlevan went on to explain, “when we wanted to begin the quality improvement project, we had no data basically…so one of the processes that we had from nine years ago was accumulating the data.”
Going beyond robust data drilldowns, Dr. Pahlevan facilitates monthly meetings with the care team to review each patient with high viral loads. Dr. Pahlevan highlighted how these efforts “give us the information on what is the most important barrier for our patient population for our viral load suppression, and then that becomes the basis for quality improvement projects for every year.” Thanks to these procedures, NUMC has seen a two percent increase in the viral suppression rate each year following the implementation of this QI project. The number of patients who were not virally suppressed went from just over 100 people in 2014 to about 20 today, with continual outreach efforts to engage anyone in the community who is not receiving care.
Using Information in Real Time
Another effective process implemented by NUMC’s leadership is rapid internal communication with all subspecialty departments in their Medical Center. Dr. Pahlevan has real-time access to viral load testing immediately after the test is processed in the hospital laboratory or any of their five to seven specialty clinics. Dr. Pahlevan explained, “I get the email, all providers become notified of the high viral load, and as soon as I get it, I talk to the case manager, to mental health, and the patient.” This has been a very effective process as the Medical Center can immediately reach out to the patients, connect them with a case manager, identify any barriers, and offer support. NUMC’s approach to care starts from robust data analysis and reporting systems. However, it is the use of data that truly contributes to their success. The staff at NUMC can reach out to patients immediately after an issue arises to check-in with them and identify and address challenges. NUMC provides in-depth, multifaceted mental health services.
“I get the email, all providers become notified of the high viral load, and as soon as I get it, I talk to the case manager, to mental health, and the patient.” Dr. Pahlevan
A significant accomplishment that NUMC takes great pride in is the Prevention of Mother to Child Transmission (PMTCT) care provided since 2003. That year there were 73 pregnant women who were HIV positive and receiving care. Dr. Pahlevan reflected how of the 73 children born, all were HIV negative: “Those kids are like 20 years old right now….and when you look at them, you feel all the satisfaction in the world by seeing those results.”
Team Effort Makes This Work
NUMC’s leadership offered some advice for new QI teams. Dr. Yasmin, Director of HIV Services at NUMC emphasized how this work needs to be a team effort and how teams need “to have belief in your project and as Martin Luther King Jr. says, take the first step in faith–you may not see the whole staircase, but you will definitely see the steps leading up to it.” The NUMC leadership team has demonstrated exemplary dedication to continually improving the care they provide and going above and beyond in supporting each patient. They accomplish this by applying lessons learned across disciplines, while still recognizing that one size does not fit all and instead use an individual approach with each patient as they strive to always improve.
The team at NUMC exemplifies great leadership and commitment to quality and we are honored to present them with CQII’s 2023 Award for Leadership in Quality Improvement.
Contact Information
Hamid Pahlevan, MD
Grant Supervisor/Counselor
[email protected]
516-572-4823
Nassau University Medical Center
Puerto Rico Ryan White Part B/ADAP Program, Puerto Rico Department of Health
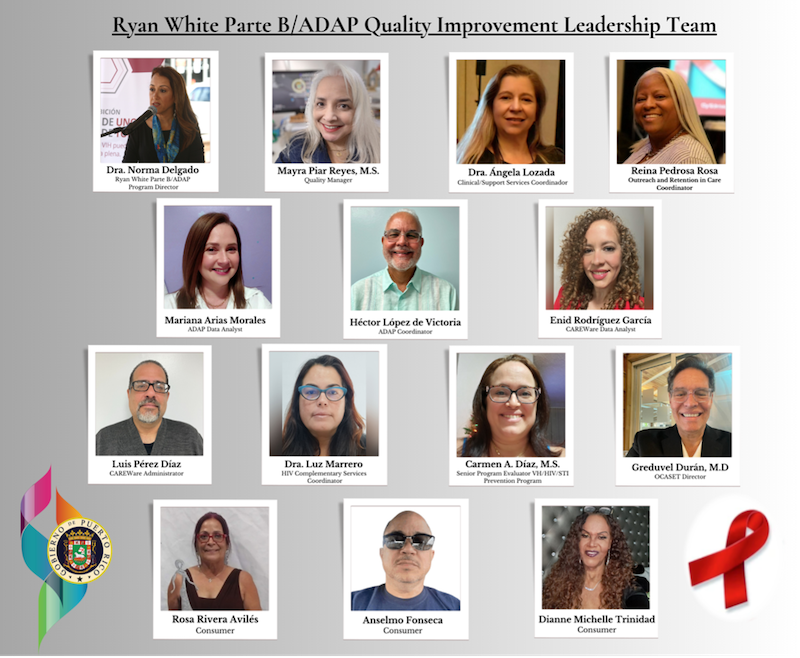
From left to right, top to bottom: Dra. Norma Delgado, Puerto Rico Ryan White Part B/ADAP Program Director, Mayra Piar Reyes, M.S., Quality Manager, Dra. Ángela Lozada, Clinical & Support Services Coordinator, Reina Pedrosa Rosa, Outreach and Retention in Care Coordinator, Mariana Arias Morales, ADAP Data Analysis, Héctor López de Victoria, ADAP Coordinator, Enid Rodríguez García, CAREWare Data Analyst, Luis Pérez Díaz, CAREWare Administrator, Dra. Luz Marrero, HIV Complementary Services Coordinator, Carmen A. Díaz, M.S., Senior Program Evaluator VH/HIV/STI Prevention Program, Greduvel Durán, M.D., M.P.H, OCASET Director, Rosa Rivera Avilés, Consumer, Anselmo Fonseca, Consumer, Dianne Michelle Trinidad, Consumer.
We congratulate the Puerto Rico Ryan White Part B/AIDS Drug Assistance Program (ADAP) for their outstanding work in quality improvement and are honored to present them with CQII’s 2023 Award for Leadership in Quality Improvement.
The Puerto Rico Ryan White Part B/ADAP Program (PRRWPBA) is housed within the Office for AIDS Affairs and Transmissible Diseases (known by its Spanish acronym as OCASET) of the Puerto Rico Department of Health (PRDOH). The PRRWPBA is responsible for the delivery of medical and support services to people with HIV throughout Puerto Rico. It is also responsible for overseeing that medical and supportive services delivered to people with HIV are of high quality; thereby, facilitating access to a comprehensive continuum of HIV care and treatment. To achieve this undertaking, the program has implemented a strong and proactive clinical quality management program (CQMP) that works directly with subrecipients, clinics, and organizations from the PRRWPBA provider network. This partnership allows PRRWPBA to exchange necessary data for performance measurement, and to inform, guide, and monitor the implementation of quality improvement (QI) activities.
The infrastructure of the CQMP is comprised of three major components: 1) the Quality Guidance Committee that leads all QI activities; 2) the Evaluation, Planning and Quality Management Unit that is responsible for generating data and evaluating systems to support decision-making processes, analyzing information obtained through these systems, and evaluating the implementation of QI processes; and 3) the Comprehensive Quality Committee comprised of all 62 Part B organizations, clinical and care centers across Puerto Rico, that constitute the Ryan White Part B providers’ network. This infrastructure has been demonstrated to be pivotal to CQMP’s effectiveness and sustainability.
Mentor Program Provides Individualized Support
In 2010, the PRRWPBA implemented the Quality Mentorship Initiative, which continues to provide individualized technical assistance to PRDOH Transmissible Diseases Prevention and Treatment Centers (known by their Spanish acronym as CPTETS) and Part B Community-Based Coordinating Agencies (CAs). Quality Mentors, along with CAREWare Managers, support CPTETS and CAs in improving skills to effectively monitor, review, and analyze their performance measurement data and identify both opportunities for and barriers to QI activities. This initiative has proven to be effective in supporting and strengthening the skills of CPTETS and CAs in implementing their QI efforts. Three QI projects were impressively implemented across all eight CPTETS focused on: 1) increasing viral suppression rates amongst people who inject drugs and youth (aged 13-24 years) with HIV; 2) increasing the number of people linked to care to within 30 days of HIV diagnosis; and 3) ensuring medical case management (MCM) plans are updated twice yearly. As a result of the hard work of the CQMP, the data reports have shown that over 12 months: 1) the viral suppression rate increased by 5.62% among youth with HIV; 2) the percent of people linked to care within 30 days of a new HIV diagnosis increased by 8.2%; and 3) patients with an updated MCM plan at least twice a year increased by 3.06%. The PRRWPBA leadership has demonstrated an obvious commitment to quality with their participation in all aspects of the QI processes.
Responding to Challenges
The PRRWPBA has faced several challenges to their QI work, particularly a lack of QI resources in Spanish and a fragmented health system: “The health system in Puerto Rico is fragmented. That means not everyone with a diagnosis with HIV will find whatever they need with one provider. And since this health system is fragmented, we have to be attentive and we have to be on top of coordinating the different services and make sure that the person will be receiving all the care that they need,” said Dr. Norma Delgado, PRRWPBA Program Director. The QI team agreed that maintaining enthusiasm and active participation of people with HIV across all levels of the CQMP and among all PRRWPBA provider networks has constituted one of their biggest challenges in their QI journey. This is mostly due to HIV-specific QI resources and trainings being in English, while Spanish is the official language in Puerto Rico. Many potential members of the QI team have been unable to participate due to materials being in English only. To address this challenge, leadership has committed time and resources to selecting and translating QI material for accessibility and improving QI understanding among people with lived experience. They are hopeful that in the future, more QI material and resources will be produced in Spanish.
Puerto Rico has also endured several natural disasters over the last six years including hurricanes, earthquakes, and most recently, the COVID-19 pandemic. Despite these challenges, PRRWPBA maintains strong engagement and care for the communities they serve by routinely reassessing and updating their emergency plans. The PRRWPBA’s Preparedness and Continuity of Operations Plan for Emergency Situations mitigates and resolves issues related to accessing medications and continuity of services, while ensuring safety and continuity of services during the aftermath of natural disasters and public health emergencies. Consequently, the PRRWPBA quality work has always been prioritized and viral load suppression rates were maintained. Access to medication was similarly never interrupted due to the strategies and actions delineated in the ADAP Emergency Contingency Plan. The ADAP Coordinator, Héctor López de Victoria, shared the importance of planning and stated that QI teams need to plan constantly, not only when emergencies arise. Héctor and the PRRWPBA team agreed that these decisions and plans must always be guided by facts, or be data driven.
One Secret to Success
Rosa, who utilizes the services offered by PRRWPBA, shared that the secret to the group’s success is empathy, and letting the community know their voices are important. The PRRWPBA shows exemplary commitment to engaging people with HIV and their voices are represented at multiple levels of involvement within the CQMP: feedback is gathered through quality committees, suggestion boxes, and roundtable groups, while workshops and educational interventions are offered to patients to increase their involvement. These individuals represent a diversity of issues and challenges faced by heterosexual women, gay, bisexual, and other men who have sex with men, and the transgender community by acting as liaisons to the community of people with HIV in Puerto Rico served by the PRRWPBA.
When community care and engagement remain at the forefront of the work, power can be leveraged, and work transformed into quality results.
When asked for words of wisdom to inform others starting their QI journey, two people with lived experiences (Rosa and Anselmo) who collaborate with PRRWPBA agreed that they let their passions drive their work. When community care and engagement remain at the forefront of the work, power can be leveraged, and work transformed into quality results. The QI team mentioned that commitment to QI must begin at the top of an organization. The importance of having a sound and strong infrastructure cannot be emphasized enough. In addition, involving people with lived experience in planning and decision-making processes constitutes one of the main lessons learned through their QI journey.
The PRDOH RWPBA team embodies true leadership and commitment to quality, and we are honored to present them with CQII’s 2023 Award for Leadership in Quality Improvement.
Contact Information
Mayra Piar Reyes, M.S.
Quality Manager
[email protected]
787-765-2929 Ext. 5109 or Ext. 5102
Puerto Rico RWHAP
Programa Ryan White Parte B/ADAP de Puerto Rico, Departamento de Salud de Puerto Rico
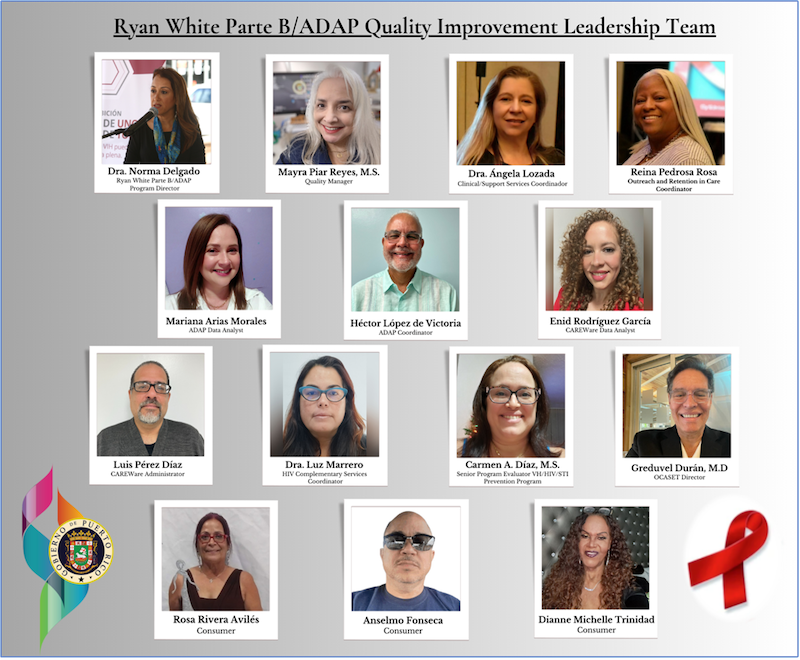
De izquierda a derecha, de arriba a abajo: Dra. Norma Delgado, Directora del Programa Ryan White Parte B/ADAP de Puerto Rico, Mayra Piar Reyes, M.S., Gerente de Calidad, Dra. Ángela Lozada, Coordinadora de Servicios Clínicos y de Apoyo, Reina Pedrosa Rosa, Coordinadora de Búsqueda y Retención en Cuidado, Mariana Arias Morales, Analista de Datos de ADAP, Héctor López de Victoria, Coordinador de ADAP, Enid Rodríguez García, Analista de Datos del CAREWare, Luis Pérez Díaz, Administrador del CAREWare , Dra. Luz Marrero, Coordinadora de Servicios Complementarios de VIH, Carmen A. Díaz, M.S., Evaluadora Senior del Programa de Prevención VH/VIH/ITS, Greduvel Durán, M.D., M.P.H, Director de OCASET, Rosa Rivera Avilés, Participante, Anselmo Fonseca, Participante, Dianne Michelle Trinidad , Participante.
El Centro para la Innovación y Mejoramiento de la Calidad (CQII, por sus siglas en inglés) se siente honrado de otorgar el Premio al Liderazgo en Mejoramiento de la Calidad 2023 al Programa Ryan White Parte B/Programa de Asistencia para Medicamentos para el SIDA (ADAP, por sus siglas en inglés) de Puerto Rico. A tal efecto, extendemos una felicitación al Programa Ryan White Parte B/ADAP, del Departamento de Salud de Puerto Rico, por su destacado trabajo en el mejoramiento de la calidad en los servicios ofrecidos a las personas con diagnóstico positivo a VIH en Puerto Rico.
El Programa Ryan White Parte B/ADAP de Puerto Rico (PRWPBA-PR) está adscrito a la Oficina para Asuntos de SIDA y Enfermedades Transmisibles (OCASET) del Departamento de Salud de Puerto Rico. El PRWPBA-PR es responsable de la prestación de servicios médicos y de apoyo a personas con diagnóstico positivo a VIH en Puerto Rico. Además, le corresponde vigilar y asegurar que los servicios médicos y de apoyo que se brinden a las personas con diagnóstico positivo a VIH en Puerto Rico sean de alta calidad; facilitando así el acceso a tratamiento y a un cuidado integral continuo para el VIH. Para lograr este objetivo, el PRWPBA-PR ha implantado un Programa de Gestión de Calidad (PGC) robusto y proactivo que rige, encamina y conduce los trabajos de mejoramiento de calidad de la red de proveedores del PRWPBA-PR mediante el desarrollo del Plan de Calidad anual del PRWPBA-PR, la implementación y seguimiento del nivel de desempeño de los indicadores de calidad monitoreados a través del Plan de Calidad anual, y el intercambio de información necesaria para determinar el cumplimiento con los objetivos establecidos en el Plan de Calidad anual y las actividades de mejoramiento de calidad. La infraestructura del PGC se compone de tres (3) componentes principales: 1) el Comité Guía de Calidad que dirige todas las actividades de mejoramiento de calidad; 2) la Unidad de Evaluación, Planificación y Calidad que se encarga de generar datos y sistemas de evaluación para apoyar los procesos de toma de decisiones, analizar la información obtenida a través de estos sistemas, y evaluar la implementación de procesos de mejoramiento de calidad; y 3) el Comité Integral de Calidad, en el que están representadas las 62 clínicas, centros clínicos y organizaciones pertenecientes a la red de proveedores del PRWPBA-PR en Puerto Rico. Esta infraestructura ha demostrado ser fundamental para la eficacia y sostenibilidad del PGC.
En el año 2010, el PRWPBA-PR implantó la Iniciativa de Mentoría de Calidad para ofrecer asistencia técnica individualizada en mejoramiento de calidad a los Centros de Prevención y Tratamiento de Enfermedades Transmisibles (CPTETs) del Departamento de Salud y a las Agencias Coordinadoras (ACs) sub-recipientes de fondos Ryan White Parte B. Los mentores de calidad, junto con los gerentes de CAREWare del PRWPBA-PR, ofrecen mentoría y apoyo a los CPTETS y las ACs en el mejoramiento de las competencias para monitorear, revisar y analizar efectivamente los informes trimestrales de ejecución y los datos relacionados a la medición del nivel de desempeño de sus respectivos indicadores de calidad; así como en la identificación de oportunidades y barreras en el mejoramiento continuo de la calidad de los servicios clínicos y de apoyo ofrecidos a las personas con diagnóstico positivo a VIH. Esta iniciativa ha demostrado ser eficaz para fortalecer las habilidades y competencias de los CPTETs y las ACs en la implementación de sus esfuerzos en la gestión de la calidad. Tres (3) proyectos de mejoramiento de calidad fueron implementados exitosamente través de los ocho (8) CPTETs adscritos al Departamento de Salud. Los mismos se enfocaron en: 1) aumentar la supresión viral en los que usuan drogas intravenosas y participantes jóvenes con VIH (de 13 a 24 años); 2) aumentar el número de personas que enlazan a cuidado médico para el VIH dentro de los 30 días posteriores al diagnóstico de infección con VIH; y 3) asegurar que los planes de cuidado de Manejo de Caso Clínico sean actualizados al menos en dos ocasiones en un periodo de un año. Como resultado del arduo trabajo del PGC, los informes de datos han demostrado que, en un periodo de 12 meses: 1) la supresión viral aumentó en 5.62% entre los participantes jóvenes con VIH: 2) el porcentaje de participantes enlazados a cuidado médico dentro de los 30 días posteriores a un nuevo diagnóstico de VIH aumentó un 8.2%: y 3) el porcentaje de participantes con un plan de cuidado de Manejo de Caso Clínico actualizado en al menos dos ocasiones en un periodo de un año aumentó en un 3.06%. La gerencia del PRWPBA-PR ha demostrado un compromiso indiscutible con la calidad mediante su participación activa en todos los aspectos de los procesos de mejoramiento de la calidad.
El PRWPBA-PR ha enfrentado varios desafíos en su trabajo de mejoramiento de calidad, incluyendo los recursos limitados sobre mejoramiento de calidad en idioma español y el fragmentado sistema de cuidado de salud de la Isla: “La isla de Puerto Rico opera dentro de un sistema de cuidado de salud fragmentado. No todos los pacientes encuentran lo que necesitan en un mismo lugar. A tal efecto, se requiere de mucha coordinación para garantizar que las personas con diagnóstico positivo a VIH reciban toda la atención y los servicios que necesitan”- dijo la Dra. Norma Delgado, Directora del Programa Ryan White Parte B/ADAP de Puerto Rico. El equipo de mejoramiento de calidad convergió en que mantener el entusiasmo y la participación activa de las personas con diagnóstico positivo de VIH en todos los niveles del Programa de Gestión de Calidad y en toda la red de proveedores del PRWPBA-PR ha constituido uno de los mayores desafíos en su travesía en el mejoramiento de calidad. Esto se debe principalmente a que los recursos y las capacitaciones sobre mejoramiento de calidad se publican sólo en idioma inglés; mientras que el idioma oficial de Puerto Rico es Español. Candidatos potenciales para representar a la comunidad de personas con diagnóstico positivo a VIH en los comités y equipos de calidad no han podido participar debido a que los materiales, guías, referencias de mejoramiento de calidad, entre otros, están disponibles sólo en idioma inglés. Debido a esto, los líderes del equipo de calidad dedican tiempo y recursos a identificar y traducir material de mejoramiento de calidad al idioma español, para que el mismo sea accesible y contribuya a mejorar la comprensión sobre el tema de mejoramiento de calidad en los representantes de la comunidad de personas con diagnóstico positivo a VIH. El PRWPBA-PR tiene la esperanza de que en un futuro haya más materiales y recursos sobre mejoramiento de calidad que se produzcan en idioma español.
Además, Puerto Rico se ha visto afectado por varios desastres naturales en los últimos seis años, incluidos huracanes, terremotos y, más recientemente, la pandemia de COVID-19. De conformidad, ha habido desafíos y retos debido a las secuelas y consecuencias de los desastres naturales y emergencias de salud pública que se han enfrentado. El PRWPBA-PR se ha mantenido en comunicación y pendiente de las necesidades y servicios requeridos por las comunidades servidas, para el cuidado del VIH, mediante la actualización y reevaluación constante de su Plan de Preparación y Continuidad de Operaciones ante Situaciones de Emergencia en caso de tormentas tropicales y huracanes, terremotos y COVID-19. La implementación de estos planes antes, durante y después de los eventos (es decir, tormentas tropicales y huracanes) ha permitido mitigar y resolver problemas relacionados con el acceso a medicamentos y servicios necesarios; pudiendo así mantener las operaciones y garantizar la accesibilidad y continuidad de los servicios durante las secuelas de dichos eventos. En consecuencia, el PRWPBA-PR siempre ha priorizado el trabajo de calidad. Los pacientes mantuvieron la supresión de la carga viral a pesar de estos eventos. Asimismo, el acceso a medicamentos nunca fue interrumpido debido a las estrategias y acciones delineadas en el Plan de Contingencia de Emergencia del Programa ADAP. Héctor López de Victoria, Coordinador del Programa ADAP, compartió la importancia de la planificación y dijo que los equipos de mejoramiento de calidad deben planificar constantemente, no sólo cuando surge una emergencia, sino también en preparación ante la incertidumbre con respecto a las secuelas y consecuencias que podrían sobrevenir. El Sr. López de Victoria y el equipo de mejoramiento de calidad del PRWPBA-PR coincidieron en que estas decisiones y planes siempre deben estar guiados por hechos o basados en datos. A pesar de estos desafíos, el PRWPBA-PR mantiene un compromiso fuerte con el mejoramiento de calidad y con el cuidado de la salud de la comunidad de personas con diagnóstico positivo a VIH a las que sirve.
Rosa, representante de la comunidad de personas con diagnóstico positivo a VIH, compartió que el secreto del éxito del grupo es la empatía y que la comunidad sepa que sus voces son importantes. El PRWPBA-PR muestra un compromiso ejemplar con involucrar a las personas con diagnóstico positivo a VIH y, por lo tanto, están representadas en todos los aspectos de la toma de decisiones dentro del Programa de Gestión de Calidad. Hay diferentes métodos a través de los cuales la comunidad de personas con diagnóstico positivo a VIH puede participar en los trabajos de mejoramiento de calidad y ofrecer retroalimentación, por ejemplo: participando como miembros de los comités de calidad regionales/locales, buzones de sugerencias, grupos de discusión. Además, se ofrecen intervenciones educativas y talleres a los participantes para aumentar su participación en los procesos relacionados a mejoramiento de calidad. Los participantes que representan la comunidad de personas con diagnóstico positivo a VIH en el equipo de mejoramiento de calidad del PRWPBA-PR ejemplifican la amplia gama de retos y desafíos que enfrentan las mujeres heterosexuales, los gay, bisexual, y hombres que tienen relaciones sexual con otros hombres, y la comunidad transgénero; actuando, a su vez, como enlace con la comunidad de personas con diagnóstico positivo a VIH que son servidas por el Programa Ryan White Parte B/ADAP en Puerto Rico. Cuando se les solicitó algunas palabras de sabiduría para otros programas u organizaciones que estén comenzando su travesía en el mejoramiento de la calidad, Rosa y Anselmo, dos participantes que colaboran con el PRWPBA-PR, coincidieron en que dejaron que su pasión impulsara su trabajo. Además, mencionaron que cuando el compromiso con el cuidado de la salud de la comunidad de personas con diagnóstico positivo a VIH permanece a la vanguardia del trabajo, aprovechamos nuestro poder y transformamos el trabajo en resultados de calidad. El equipo mencionó que el compromiso con el mejoramiento de calidad debe comenzar en el tope con el nivel gerencial de su organización. La importancia de contar con una infraestructura de calidad sólida, no se puede enfatizar lo suficiente. Además, indicaron que involucrar a los participantes en los procesos de planificación y toma de decisiones constituye una de las principales lecciones aprendidas a lo largo de nuestra travesía en el mejoramiento de calidad.
El equipo del PRWPBA-PR ejemplifica un verdadero liderato y compromiso con la calidad, y tenemos el honor de presentarles el Premio de CQII al Liderazgo en el Mejoramiento de la Calidad 2023.
Información del contacto
Mayra Piar Reyes, M.S.
Gerente de Calidad
[email protected]
787-765-2929 Ext. 5109 o extensión. 5102
Puerto Rico RWHAP
Tarrant County HIV Administrative Agency, TX

From left to right, top to bottom: Jonathan Ford-Community Engagement Specialist, Lisa Muttiah-HIV Grants Manager, S. Renee Thomas-Grants and Data Coordinator, Barbara Kakembo-Financial Coordinator, Rasheda Bell-Data Analyst, Dulce Lozano-Assistant Financial Analyst, Lonnetta Wilson-HIV Initiatives Program Manager, Kaitlyn Malec-Assistant Quality and Planning Coordinator, Glenda Caballero Lewis-Administrative Assistant, Kaitlin López-Grant Coordinator Quality and Planning.
We congratulate Tarrant County HIV Administrative Agency (TC HIV AA) for their outstanding work in quality improvement (QI) and we are honored to present them with CQII’s 2023 Award for Leadership in Quality Improvement.
TC HIV AA manages all funding for HIV care and services in the North Central Texas area. The service region includes the Ryan White HIV AIDS Program (RWHAP) Part A Fort Worth-Arlington Transitional Grant Area (TGA) and a RWHAP Part B Health Service Delivery Area (HSDA), and is a recipient for RWHAP Parts C and D, Ending the HIV Epidemic in the U.S. (EHE), and Housing Opportunities for People With AIDS (HOPWA). The agency provides direct technical assistance to their grant subrecipients on a range of QI topics including capacity building, care coordination, and linkage and retention in care. They assist their subrecipients in developing their own quality management plans and projects and connect them to resources and trainings. The TC HIV AA has consistently championed QI projects for innovation and change across North Central Texas for more than 30 years.
Expanding Consumer Involvement in CQM
The TC HIV AA Clinical Quality Management (CQM) program consists of key leadership staff and a robust CQM committee. The TC HIV AA’s CQM program has relied on the insights of people with HIV to inform their QI work. While some organizations face challenges in meaningfully involving people with HIV, especially after the COVID-19 public health emergency, TC HIV AA has been successful in rebuilding their Community Advisory Board (CAB) named the Health Improvement Team (or HIT HIV), which aims to create resources for people with HIV by people with HIV. TC HIV AA’s approach to rebuilding the CAB included investing in the community’s participation by supporting CAB member’s QI training and leadership development through a variety of internal and external training including Training Consumers in Quality (TCQ) and Building Leaders of Color (BLOC). The leadership team has also shared techniques used and lessons learned with their subrecipient agencies to encourage effective engagement of people with lived experience at all levels.
Kaitlin Lopez, Grants, Quality & Planning Coordinator, emphasized the value of “being able to find a trusted member of the community that can then go back out into the community and say, 'look, this is our mission, you can trust me, and we can trust this organization to help improve the lives of those living with HIV.'" This investment in the community has been an immensely rewarding experience for the TC HIV AA leadership team as they saw community champions develop into leaders beyond the organization. One individual later joined the Texas state quality management committee, and many have represented HIT HIV at national trainings and conferences.
The TC HIV AA’s commitment to community engagement has provided the CQM program with valuable insights on areas of focus for improvement of their initiatives. While data trends initially alerted them to the issue, information from listening sessions with people with HIV helped the team truly understand the need and urgency of implementing a rapid start ART program. Kaitlin Lopez reflected that “those were quality insights that really inspired those changes and now you have this innovative program that’s in an emergency department (ED), one of the ED’s that serves or diagnoses the most individuals living with HIV.”
Training Secures Buy-in, Prepares Staff
While the TC HIV AA has had many achievements in QI, they have still faced challenges in their QI journey. Lisa Muttiah, HIV Grants Manager for the TC HIV AA, pointed to establishing subrecipient staff buy-in as an initial challenge faced by the CQM team in their quality work. She went on to describe the efforts made by the TC HIV AA QI team in “really helping people understand how quality leads to improved health outcomes. We’re not trying to do busy work; we’re trying to do meaningful work.” Lisa emphasized how the vision of their QI work starts with having committed and competent staff that truly understand and are passionate in the power of quality.
When you are new to the QI space, “don’t be afraid to ask questions." Kaitlyn Malec, Assistant Quality and Planning Coordinator
The TC HIV AA leadership utilizes a variety of internal and external training resources to build on the QI resources and capacity in their subrecipient organizations. The leadership team highlighted the use of Life QI as a tool to allow subrecipients to tangibly track their Plan-Do-Study-Act (PDSA) cycles and understand their data. IHI Open School is also made available to all subrecipient agencies with trainings on new methodologies such as Lean Six Sigma. Lisa Muttiah went on to highlight how the secondary value of sharing these resources with subrecipient agencies is the “peer-to-peer learning component of it because this information is shared within the quality management committee and there is a little bit of pressure if one organization is able to do something and make an impact well – that may make another organization want to step it up.”
When asked for “words of wisdom” gained through their experience, Kaitlyn Malec, Assistant Quality and Planning Coordinator, emphasized that when you are new to the QI space, “don’t be afraid to ask questions – there’s listservs and there’s so many amazing people that are dedicated, so don’t be afraid.” Going past trainings and technical assistance, Kaitlin Lopez also highlights the importance of building a strong team by “finding those champions in the community and finding those trainers that have been doing this for a while that can help to build something uniquely different to your jurisdiction.”
The TC HIV AA leadership has demonstrated a consistent commitment to quality through projects that involve multiple community stakeholders and subrecipients. The leadership team emphasizes empowering and guiding both subrecipient agencies and their community with access to a robust catalog of trainings. By investing in staff and community, the TC HIV AA has seen tremendous success in the impact and retention of their initiatives.
The team at TC HIV AA exemplifies great leadership and commitment to quality and we are honored to present them with CQII’s 2023 Award for Leadership in Quality Improvement.
Contact Information
Kaitlin Lopez
Grant Coordinator, Quality & Planning
[email protected]
817-370-4526
BeatHIVTC.org
2022 Quality Awards
Dallas County Health & Human Services HIV Administrative Agency, Dallas, TX

DCHHS staff from left to right: Regina Waits, CD CQM Health Advisor; Dr. Philip Huang, Director/Health Authority; Sonya Hughes, Ryan White Grants Compliance Assistant Director; Dr. Oscar R. Salinas, CQM Program Coordinator; Angi Jones, Clinical Quality Management Advisor
Coaches from top to bottom: Michael Hager, President & CEO of Hager Health LLC; Jamie Shank, President & CEO of Organizational Empowerment LLC
We congratulate the Dallas County Health & Human Services (DCHHS) HIV Administrative Agency (AA) for their outstanding work in quality improvement, and we are honored to present them with the Center for Quality Improvement and Innovation’s 2022 Award for Leadership in Quality Improvement.
Based in Dallas, Texas, DCHHS is responsible for the health of over 2.6 million Dallas County residents and serves around 24,000 people with HIV, and a little more than half of them are receiving Ryan White HIV/AIDS Program (RWHAP) services. For the first time, the AA Clinical Quality Management (CQM) team brings subrecipients providing RWHAP services in the Dallas Eligible Metropolitan Area (EMA) and the Dallas and Sherman-Denison HIV Service Delivery Areas (HSDA) together to work on a joint project focusing on people out of care or at risk of falling out of care. The outpatient ambulatory health services provider data shows clients were missing more than 20% of scheduled HIV-related medical appointments over a 12-month period during 2019; each of the eleven funded subrecipients developed their own plans aligned to assist in the regional “Return to Care” (R2Care) Region-wide Quality Improvement Project, focusing on what they could do in their agency based on the services they provide and the challenges they identified to improve retention in care. “Bringing all the pieces together and aligning the community, in any setting, with lots of different players and activities can be difficult, but this is important, and we appreciate the impact this has had on getting everyone on the same page and getting everyone working towards the same goal,” said Philip Huang, MD, MPH, Director of DCHHS.
“My advice would be to break it up into different pieces, so you are not overwhelmed, and respect and be kind to one another even if there are differences of opinion.”
Sonya Hughes, Assistant Director, DCHHS
The interventions have varied from incorporating follow-up by case managers into appointment reminders at Community Dental Care, to reducing the client of burden of the eligibility process with a virtual 6-month attestation using the EMR at Parkland Health. “It can be overwhelming at first, all the components of a Ryan White Program,” said Sonya Hughes, Assistant Director, “My advice would be to break it up into different pieces, so you are not overwhelmed, and respect and be kind to one another even if there are differences of opinion.” AIDS Services of Dallas has worked to improve rates of permanent housing for clients exiting their transitional housing program through promoting financial independence in these clients with vocational training, assistance applying for disability if needed, and addressing the substance use and mental health challenges of their clients. Prism Health of North Texas is working on decreasing no show rates by utilizing tablets to improve retention in care of transgender women, while AIDS Healthcare Foundation and the Resource Center have sought to increase retention through the provision of tablets to target subpopulations affected by language barriers. Health Services of North Texas has improved their data collection, revised their phone system, and participates in monthly care coordination and daily huddles to identify and re-engage clients out of care. Callie Clinic has implemented an “Undetectables Program” to improve viral suppression rates by adding mental health services, offering incentives, and focused trainings for case managers. “As a person living with HIV, I’m particularly excited and encouraged by the work that we’ve done to enhance community inputs and engagement,” said Michael Hager, MPH, MA President and CEO of Hager Health and consultant to the DCHHS team. Legacy Cares is working on improving rates of successful intake appointments by increasing appointment reminders, completing client paperwork in advance to ease client burden, and holding staff debriefs on clients (who miss over 40% of sessions), on what could be improved. To manage all of these interventions, the DCHHS CQM committee has developed standardized reporting forms and a calendar for each agency to use to report their individual progress each month. When asked what their greatest challenge has been during this quality improvement (QI) journey, Oscar Salinas, MD, the CQM Program Coordinator, likened it to “building the plane while flying it… Change has to start with ourselves, educating ourselves, and exporting the concepts of CQM culture as a journey where all of us have room for participation to the subrecipients.”
Establishing a culture of quality across eleven subrecipients, each with different services and challenges, is no easy feat. “The team focused on ALL components of CQM: infrastructure, performance measurement, QI, in concert with one another versus as separate ‘tasks’ or concepts, and the team modeled what was expected of subrecipients and what makes an impactful program,” said Jamie Shank, MPH, CEO of Organizational Empowerment and consultant to DCHHS, and leading by example was a significant facilitator in their success. The teamwork on the DCHHS is palpable, and the people they serve are always centered in their work: “We talk about why a lot, but they are the who. In the process of making sure quality and quality improvement are well understood, we are trying to make things better, more efficient,” said Angi Jones, MBA, a CQM Advisor, “These are people, and we are trying to improve the quality of their life.”
Contact Information
Oscar R. Salinas, MD
[email protected]
214-819-1856
Santa Rosa Community Health Centers, Santa Rosa, CA
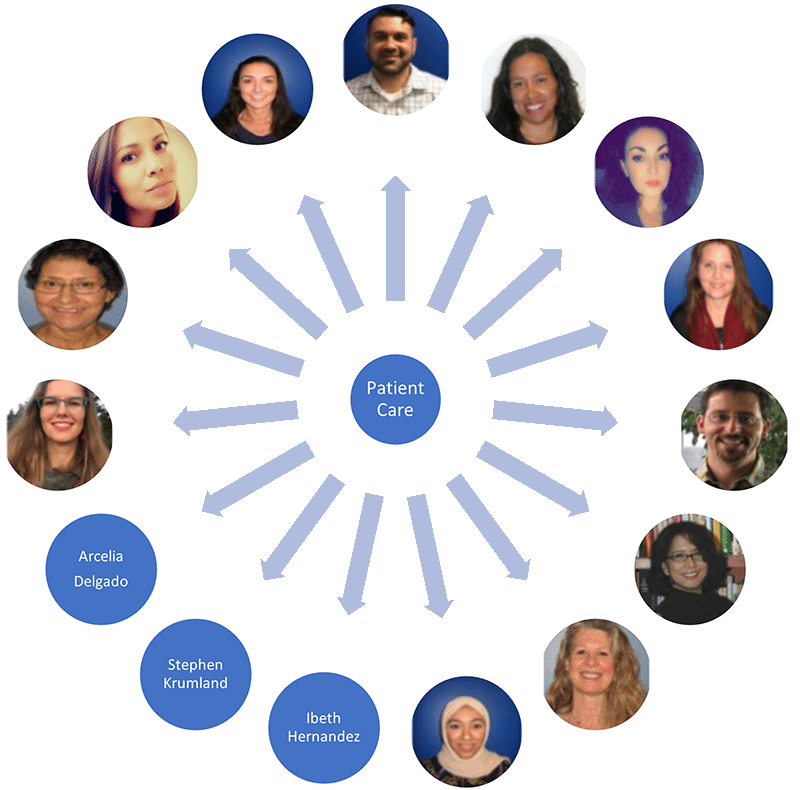
From top center, clockwise: Ben Leroi, Special Population Programs Director; Paola Diaz, VIDA Program Manager; Paloma Blair, VIDA Program Specialist; Angela Walker, Pharmacy Support Specialist; Dr. Daniel Toub, VIDA Clinician; Dr. Ele Lozares-Lewis, VIDA Clinician Lead; Ilka DeGast, VIDA Psychologist; Mona Alsaffar, VIDA Sr. Quality Specialist; Ibeth Hernandez, Medical Assistant; Dr. Stephen Krumland, Clinician; Arcelia Delgado, RN Case Manager; Nadya Hristeva, VIDA Clinical Pharmacist; Judith Brazis, ADAP and Access Coordinator; Patricia Ibarra, VIDA Clinical Team Assistant; and Rose Lapierre, RN Case Manager.
We congratulate Team VIDA at Santa Rosa Community Health Centers for their outstanding work in quality improvement and we are honored to present them with the Center for Quality Improvement and Innovation’s 2022 Award for Leadership in Quality Improvement.
Santa Rosa Community Health Centers (SRCHC) are located in Santa Rosa, California and offer integrated services including primary, pediatric, and mental health care. Team VIDA is the HIV team within SRCHC and includes programmatic staff as well as case managers, clinicians, pharmacy staff, and a quality coordinator. In the fall of 2020, the California Department of Public Health (CDPH) began a quality improvement (QI) initiative to increase the number of Ryan White HIV/AIDS Program (RWHAP) clients receiving comprehensive healthcare coverage (CHC). Team VIDA increased the number of clients receiving non-medical case management who are enrolled in CHC from 58% to 93%, well surpassing the statewide goal of 85%, in just six months. But their QI journey has not always been easy. After one of their largest clinics was affected by the 2017 California wildfires, Paola Diaz, HIV Operations Manager, said she “was challenged to think about how our patients would get care and think about what barriers they would face. This process didn’t start off as a QI project, but more so as a necessity of the time.”
To achieve such impressive results, first an overhaul of the data collection process was in order. “Data wasn’t being collected the same way everywhere, and we had to review our data and validate it until we were comfortable that it was complete and correct, to start moving forward with a project,” said Paola. When the RWHAP Part B Clinical Quality Management (CQM) Program identified CHC as a priority QI project, Team VIDA staff immediately reviewed their data and engaged with CDPH staff on methods to improve data collection in its central data system, ARIES. Team VIDA also utilized data reports that identified clients who were uninsured and may need a follow-up. Team VIDA began discussing the CHC performance measurement outcomes at their monthly quality meetings. All clinic staff including management/administrators, clinicians, and support staff attended these meetings. With just a data team of two, consisting of Paola and Mona Alsaffar (HIV Sr. Quality Specialist), they were able to restructure their data collection process to ensure data completeness and accuracy. After conducting a process mapping activity with the RWHAP Part B CQM Program, Team VIDA established an AIDS Drug Assistance Program (ADAP) and Access Coordinator (ACC) role. This individual is trained to have expertise on ADAP, and all health insurance matters for people with HIV in California and in the local region. The ACC is known by all clinic staff and community partners, and the process for connecting clients to the ACC is built into the clinic workflows. Once the ACC connects with the client, there is another well streamlined process that ensures that a client is set up with an appropriate CHC option. What can often take other providers several days or even weeks to complete, Team VIDA has streamlined into a process that can be completed in less than an hour.
We’re like a family, so when we do a project, we like to work with each other and that makes the work fun and exciting.
Mona Alsaffar, HIV Sr. Quality Specialist
The culture of quality at Team VIDA is ubiquitous. New staff receive quality training to ensure everyone is familiar and engaged with QI terms and methodology, and all staff receive cross-training to fortify the team’s workflow, which was a lifesaver during the height of the COVID-19 pandemic. Team VIDA management has fostered not only a culture of quality, but also a culture of trust, communication, and recognition: “They always give you time, encourage you, remind you of the main goal, and they form a connection with every coworker. We’re like a family, so when we do a project, we like to work with each other and that makes the work fun and exciting,” said Mona, who also uses games like jeopardy to motivate staff and keep their QI knowledge fresh.
When asked if they had any words of wisdom to share for people just starting out on their own QI journeys, Paola had this to say: “We don’t own the project, the team owns the project. We are all responsible to make sure the work gets done the best it can. When everybody felt that they were part of a project, it became easier. If we keep everyone focused on the goal, we get better patient care, we get better results.”
Contact Information
Paola Diaz, HIV Program Manager
[email protected]
707-483-6128
2021 Quality Awards
Southeast Mississippi Rural Health Initiative, Inc. (SeMRHI), Hattiesburg, Mississippi

We congratulate Southeast Mississippi Rural Health Initiative, Inc. (SeMRHI) for their outstanding work around improving their viral suppression rates. We are honored to present them with CQII’s 2021 Award for Measurable Improvements in HIV Care to Mitigate HIV Disparities.
SeMHRI is a network of federally qualified health centers (FQHCs), which provides integrated primary, HIV, and behavioral health care services for people with HIV in southern Mississippi. With 5 school-based health centers, they provide HIV education, prevention, and testing for youth. “What I’m most proud of are the patients,” said Tonya Green, the Director of Social Services and Ryan White Program Coordinator at SeMRHI’s Hattiesburg Family Health Center. “I’m really proud of their willingness to get into care and being proactive in their health care despite all of the stigma. We could not do what we do without these young patients being engaged, open minded, and trustworthy of us in this journey they’re going through.”
SeMRHI participated in CQII’s past two collaboratives (end+disparities Collaborative and create+equity Collaborative) and used data-driven quality improvement techniques to identify youth who are not virally suppressed or have missed appointments. Medical case managers used a patient checklist to identify and address barriers to antiretroviral therapy (ART) and medical care adherence. ‘Health literacy illustration’ tools were used to visually help youth understand the effects of ART on viral suppression rates. SeMRHI’s goals of this intervention included to improve youth outreach, especially to those who were not virally suppressed; identify barriers to care and make appropriate referrals; increase health literacy; manage mental and substance use issues affecting youth; and ensure consistent follow-up on missed appointments.
This intervention was successful in improving viral suppression rates for youth, defined as ages 13 through 24. Over a 12-month period from July 2018 to June 2019, viral suppression rates for youth increased from 58% to 78%. The viral suppression rates for youth continue to be sustained at rates at or above 75%. As of April 2021, the current viral suppression rate for youth ages 13-24 was 77%. As a result of this intervention’s success, it has now been implemented for patients of all ages, not exclusively for youth patients.
This is not to say that SeMRHI did not face any challenges along the way. COVID-19 brought about unprecedented barriers to the work they do. “COVID-19 really mirrors HIV,” reflected Tonya. “The treatment and the guidelines were constantly changing, just like when HIV came out. The greatest challenge was having to wrap our head around what is COVID-19 and how we can educate our patients on ongoing safety measures.” Through the pandemic, SeMRHI succeeded in introducing a virtual consumer advisory board and through this, they were able to provide patients with peer support and education about COVID-19.
Some words of wisdom Tonya gives for other providers is to find your niche. “If you could do something for free for the rest of your life that makes you happy, that is your passion,” emphasized Tonya. “My passion is in HIV care, and I really love what I do.”
Contact Information
Southeast Mississippi Rural Health Initiative, Inc. (SeMRHI)
Tonya Green, Director of Social Services
[email protected]
601-582-2619
Khalil Hassam, DC Health, HIV/AIDS, Hepatitis, STD and TB Administration, Washington, DC

We congratulate Khalil Hassam for his outstanding leadership in quality improvement (QI), and we are honored to present him with CQII’s 2021 Award for Leadership in Quality Improvement.
Over the past decade and a half, Khalil has been dedicated to quality improvement on the local, regional, and national level. In his current role as the Clinical Quality Improvement Specialist at DC Health, he has implemented effective and sustainable clinical quality management programs, innovative QI initiatives with measurable results that have benefited HIV clients and regional improvement efforts to work across a network of HIV organizations.
Khalil was the primary convener in bringing senior leaders together to replicate the long-term success of the DC Collaborative and the DC Eligible Metropolitan Area (EMA) Ryan White HIV/AIDS Program throughout the HIV/AIDS, Hepatitis, STD and TB Administration (HAHSTA). His work resulted in an organizational shift to advance clinical quality management infrastructures, including standardized QI curriculum for all new hires. Khalil was also the visionary of establishing a “culture of quality” in both DC Health and HAHSTA by embracing a middle-out approach that continues to inspire senior leaders, front-line staff, and persons with lived experiences receiving HIV services. He promoted the regional use of new QI methodologies and tools by making these concepts simpler and more accessible for all subrecipients with the EMA.
In his role as the DC Collaborative co-lead and the driving force behind the #DCALLCAPS end+disparities Collaborative team, Khalil helped improve health outcomes and lessened disparities among Transgender and Youth focus populations; see chart below. He designed a novel quality-driven business model, which combines grants with a value-based reimbursement model. With lean methodology as his driving force, Khalil led a Kaizen group to reduce complexity for subrecipients. Khalil was also a key quality leader in HAHSTA’s Rapid ART systems level change. He is a highly effective QI coach for his subrecipients and frequently uses games and simulations to encourage participation and problem-solving. He is able to optimize limited QI resources to their full potential, while also using his sphere of influence to advocate for additional quality resources.
Khalil seeks to dismantle the notion that QI is overly structured. He encourages people to focus on the personal aspect of quality, not only to improve understanding of QI methodologies, but also to improve their own life. “Quality is about how you unload your dishwasher, it’s about how you send your emails, your commute to work, and so getting folks to think about quality as a way to enhance and better their own life is more digestible than ‘we’re all going to engage in this PDSA cycle so that we can reduce the grant monitoring time,’” said Khalil. He hopes to one day “work himself out of a job,” when a culture of quality is so ubiquitous that QI becomes obsolete.
When asked what lessons he learned at the start of his career that he still uses every day, Khalil replied “When you see an opportunity, go in, and produce, and create value. If you see an opportunity to improve something, don’t wait; step into the void and start making value wherever you can.”
Contact Information
Khalil Hassam
[email protected]
202-727-5659
Reachelian Ellison, The Houston Regional HIV/AIDS Resource Group, Inc., Houston, Texas

We congratulate Reachelian Ellison for her outstanding work in consumer engagement, and we are honored to present her with CQII’s 2021 Award for Consumer Engagement in Quality Improvement.
As the Consumer Relations Coordinator at The Houston Regional HIV/AIDS Resource Group (TRG), located in Houston, Texas, Reachelian has revolutionized TRG’s ability to deliver quality care and enable services for people with HIV in and around Houston by implementing a Consumer Engagement Program, the Healthy U Initiative, and an “Education First” approach.
“Nobody wants to be in a one-sided relationship.” This is Reachelian’s mantra behind the restructuring of TRG’s consumer engagement program. Before Reachelian joined TRG, people with HIV were only engaged in one regional consumer advisory board. Reachelian implemented agency-specific consumer advisory boards (CABs) at every subrecipient and created a support structure that identified a CAB liaison and CAB chair who work in tandem to collect the experiences and concerns of people with HIV. Reachelian also helped split Houston Regional’s 51 counties into 4 regional CABs, which have been better suited to address the variety of consumers’ geographic areas and their needs. Reachelian conducts annual subrecipient consumer involvement monitoring visits and reports these results to the Ryan White Planning Council Quality Improvement Committee, local stakeholder agencies, and local consumer organizations.
Reachelian’s Consumer Engagement Program trained and supported people with HIV to become more actively involved in community stakeholder groups, as well as achieve their personal goals. Her program gave people with HIV the platform, resources, and support to become more empowered in seeking care and as advocates. Her Healthy U Initiative, based on the Experienced Based Co-Design Model (EBCD), calls on consumers (in collaboration with their clinical providers) to design educational materials for their peers for clinical sites. These deliverables helped improve patient compliance and information accessibility.
Reachelian’s “Education First” approach ensures that consumers know the purpose of any meeting they attend and what their role at the table is, which ensures consumers are equal partners in improving HIV care: “This has made a huge difference for me in being able to find consumers to participate, because then they’re not being called out to everything or things that they’re not interested in. It’s more of a focus on ‘what do you want me to call you about’ versus ‘there’s a meeting and we want warm bodies’,” said Reachelian.
Reachelian recognizes that each consumer brings their own unique experiences and abilities to the table by “meeting people where they are.” This allows for a relationship of trust and mutual enrichment between providers and consumers. Citing the diversity of the population of people with HIV, Reachelian understands that a one-size-fits-all approach to consumer engagement will not be successful: “There is a disconnect between staff seeing clients as having any real type of value to the agency beyond being a consumer. There needs to be more appreciation of the differences because a lot of the clients have skills that are overlooked or undervalued.” It is a testament to Reachelian’s stewardship that several consumers she has worked with have gone on to pursue higher degrees and higher positions within the CABs.
Contact Information
Reachelian Ellison
[email protected]
832-533-0743
2019 Quality Awards
Ryan White Wellness Center, Roper St. Francis Healthcare, Charleston, South Carolina

Susan Berry & Doug Seymour from The Ryan White Wellness Center, South Carolina.
The Ryan White Wellness Center uses peer navigators to provide an additional level of support to clients that face challenges remaining in care and achieving viral suppression. The peer navigators began their work in early 2016. The navigators worked closely with the clinical case management team and administrative staff to create policies and procedures and develop peer-led strategies. Navigators provide various services to clients including: personalized reminder calls, follow-ups after visits, regular check-ins by telephone, and enhanced, peer-led treatment adherence counseling.
Over the course of the program the role of the navigators was expanded to include housing assistance, job readiness, and aging with HIV. At the inception of the peer navigation program the retention rate among clients referred to the program was 78 percent and the viral suppression rate was 47 percent. At the end of 2017, the viral suppression rate among those clients was at 77 percent and the retention rate was 94 percent.
Trillium Health, Rochester, New York
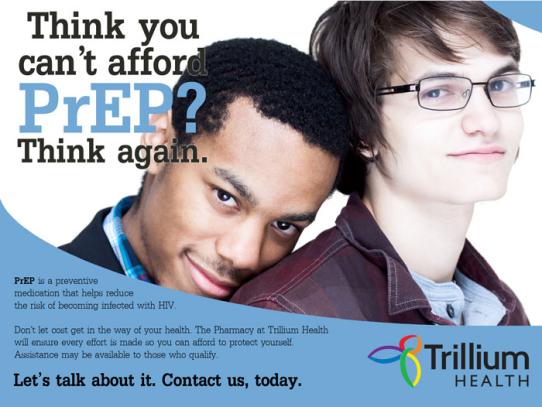
Trillium Health is an independent, neighborhood health center that has been providing comprehensive HIV care since 1989. Trillium made a concerted effort to reach out to individual not yet engaged in care. They launched a PrEP-Plus program that now has over 600 clients (one of the largest in New York State). While PrEP is not funded by Ryan White HIV/AIDS Program dollars, this outreach effort led to improvements throughout the patient population. The program started by identifying social group leaders and influencers to begin treatment and encourage people in their social and sexual networks to do the same.
These efforts were supported by an extensive marketing campaign using social media. This guerilla outreach/marketing team is made up of young men who have sex with men who conduct outreach at various venues and digital outreach using mobile phone dating apps. Using sound quality improvement methodology, they saw the need to improve the rates of the undiagnosed. Those individuals interested in beginning treatment were immediately linked to an intake specialist to facilitate the beginning of treatment. Before this guerilla market team was announced, Trillium patients were virally suppressed in 136 days on average.
This campaign led to patient's being virally suppressed in 58 days. To date, all newly diagnosed individuals identified by the guerilla/outreach team have begun antiretroviral treatment. Trillium attributes this success to their sex-positive approach and the trusting relationships built during outreach interactions. The team quickly discovered that they were identifying more undiagnosed HIV infection and acute HIV infection compared to Trillium's traditional, walk-in HIV testing.
Alabama Quality Management Group
Since 2006, Ryan White HIV/AIDS Program (RWHAP) recipients in Alabama have been meeting to share ideas on how to ensure optimal health for people living with HIV. The Alabama Quality Management Group (AQMG) initially included Part C and D recipients but over time, was expanded to also include Part B providers and now functions as a cross-Part collaboration. Members represent organizations providing services across the entire state-all 67 counties.
The group's priorities currently focus on 1) viral suppression; 2) retention in care; and 3) engaging new patients in care. The group assisted the Alabama Department of Public Health's Surveillance Branch with the implementation of the Data 2 Care Project. Data 2 Care assists RWHAP recipients in obtaining demographic data for clients who are truly out of care so that efforts can be focused on the re-engagement of those clients. In addition, the group is focusing on no show rates.
Members are collecting data on the percentage of patients who are a no show for at least one HIV-specific medical visit. This priority grew out of research conducted at the University of Alabama, Birmingham's 1917 Clinic showing that patients who missed visits within the first year after initiating treatment for HIV were at higher risk of dying than patients who attended all scheduled appointments. The group has secured funding for a statewide Data 4 Care intervention focused on reducing no-show rates. These activities will be initiated later this year.
Broward County EMA Ryan White Part A Clinical Quality Management (CQM) Program
The Fort Lauderdale/Broward County EMA established a system-wide quality assurance and continuous quality improvement program in 1997. A major project of the CQM program was the Consumer Health Experience Initiative (CHEI) to assess the quality of service delivery in the EMA by evaluating the client experience. A consultant gathered qualitative and quantitative data through a "secret shopper" experience at all subrecipients. Additionally, two educational modules to engage all subrecipient agencies and staff were conducted. Module One, "Creating a Welcoming and Responsive Service Environment for People Living with HIV," focused on identifying customer service themes of person-centered care, cultural humility, conscious and unconscious biases, and motivational interviewing.
Module Two, "Quality Initiative to Improve Customer Service and Care to People Living with HIV in Broward County Florida," aggregated mystery shopper/consumer experiences, identified facilitators/barriers to care, reviewed Module One evaluation data, and identified interventions to improve client engagement in services. Each agency received a final assessment of their results from the mystery shopper assessment, team culture survey, and Module One evaluation. In response to the findings, the CQM program is working to remove the barriers to care identified by the CHEI.
Orange County Health Care Agency, 17th Street Testing, Treatment, and Care Clinic
The California Ryan White Part B Clinical Quality Management (CQM) program, in conjunction with the California Prevention Training Center (CAPTC), implemented a quality improvement pilot program to increase extragenital gonorrhea and chlamydia (GC/CT) screening in two high-volume Ryan White Part B clinics. One of the selected sites was Orange County Health Care Agency's 17th Street Testing, Treatment, and Care Clinic, a county public health clinic.
The primary goal of the pilot project was to improve sexually transmitted disease (STD) screening for men who have sex with men who are living with HIV. The clinic sought to increase extragenital screening by giving patients an option to self-collect swabs for pharyngeal and rectal gonorrhea and chlamydia. This option required the clinic to conduct a validation study for patient self-collected swabs. To ensure practice transformation, the clinic assigned a dedicated staff person to liaison with all stakeholders and staff. Patient input on self-collection procedures was obtained during the pilot project--patients were pleased with the new self-collection procedures.
The clinic is now in the process of finalizing and formalizing its new screening protocols, including configuration of the electronic medical record to allow electronic lab ordering and processing of patient-collected samples. Lessons learned from the implementation of this pilot have been valuable in framing how the California Department of Public Health will continue to support STD screenings for people living with HIV.
Marisa McLaughlin, Senior Specialist for Quality and Performance Improvement, Portland TGA
An example of Marisa McLaughlin's leadership has been her work to expand technical assistance provided by HIV Care Services (HCS) around the development of contractors' annual Clinical Quality Improvement (CQI) Plans. In response to needs expressed by contractors related to the CQI plans, Marisa developed and implemented an annual review of contractor performance measurement and quality management. The goal of this annual review is twofold, to assist with the development of CQI plans and to increase awareness and engagement in the review of programmatic data.
The reviews also solidify the role of HCS as a source of expertise, collaboration, and support to contractors to create sound evidence-informed quality goals. Marisa has also been leading the development of the Viral Suppression Support Project in the Portland-Multnomah County TGA. Obtaining viral load laboratory results from state surveillance is a new endeavor for the TGA. Marisa worked to ensure providers had clear direction for conducting outreach to clients that are not virally suppressed or are out of care. She ensured that people living with HIV were involved in the project. The discussions resulted in a draft work plan identifying which service providers would be first to reach out to clients and work with them toward viral suppression or stronger medical engagement.
Neighborhood Health Services Corporation
To address sub-optimal medical appointment adherence (based on 2016 year-end statistics) the Neighborhood Health Services Corporation and its Early Intervention Program, in conjunction with its Consumer Advisory Board (CAB), designed and carried out a quality improvement project to address the sub-optimal adherence to appointment rates. The group committed to develop a quality improvement project based on this data to increase the adherence rate to 80%. They developed a tool to assess reasons for non-adherence, analyzed the results and then developed an improvement project using Plan-Do-Study-Act Cycles to test their interventions.
2017 Quality Awards
Maricopa County Phoenix EMA

Phoenix/Maricopa County EMA Staff
RWHAP clients have far better HIV outcomes than those not getting Ryan White care, according to HRSA's client level RSR data system. The Maricopa (Phoenix) metropolitan area RWHAP Part A grant recipient is but one example, having achieved a 7% jump in viral suppression across the Eligible Metropolitan Area (EMA) grant coverage area. Maricopa's results are an outcome of multiple planning efforts and their application of various quality improvement resources, like the well-known PDSA cycle or the NQC Disparities Calculator that was used to identify population disparities to then develop staff and service needs in response.
Linda Despines, University of Pittsburg Medical Center

Linda Despines - University of Pittsburg Medical Center
Sixteen years. Seemingly countless quality improvement projects. And a few handfuls of awards. Linda Despines has been a robust user of the HRSA HIV/AIDS Bureau's extensive quality improvement resources, from HAB's HIV performance measures to HIVQUAL to the CAREWare data software program as well as NQC's national technical assistance program. Despine also directed a project that realized a significant improvement in documented receipt of oral health care by HIV patients at PACT.
Dawn Trotter, Evergreen Health Services

Dawn Trotter - Evergreen Health Services
There is no job title for Peer Extraordinaire. Yet. Dawn Trotter of Buffalo's Evergreen Health Services (real job title: Peer Retention Support Assistant) delivers peer services in her agency and somehow participates in numerous advisory boards focused on consumer involvement and quality improvement. All this and she got 30 HIV patients back in care over the last 6 months.
Randall Furrow, Maricopa County Phoenix EMA
Randall Furrow, Maricopa County - Phoenix EMA
Randall Furrow has worn, as they say, many hats during his time working on the Phoenix Ryan White planning council. He started as a member in 2004 and later became Chair, simultaneously working on enhancing consumer involvement in planning and quality improvement as well as more robust patient self-management.
2016 Quality Awards
Nationwide Childrens' Hospital, FACES Quality Improvement Committee
The Family AIDS Clinic and Education Services (FACES) program at Nationwide Children's Hospital is central Ohio's primary HIV clinic, serving more than 400 HIV-infected clients in more than 40 counties. The program's quality improvement committee (QIC) was recognized for their successful implementation of a "stoplight project" focused on increasing viral suppression. The project aimed to get as many clients as possible to an undetectable viral load (≤ 40) level. This target is much lower than the 200 copy/ml threshold required for HRSA reporting.
The QIC meets twice a month to review viral load data for each client, particularly those for clients in the "red light" category (load >1000 copies/ml) and clients with a viral load showing evidence of a loss of virologic control. Each client is discussed and individualized multidisciplinary care plans are developed.
Through a review of the patient population, the QIC identified three key drivers that prevented achievement of viral suppression-mental illness, non-compliance with medications, and failure to show up for appointments. Interventions were developed in response to each driver. For example, the interventions related to no shows included reminder calls to patients 48 hours prior to an appointment to make sure the client can arrange transportation with their insurance company and calls by peer navigators within 24-48 hours of a missed appointment.
Since the project was initiated in 2013, the viral suppression rates have increased significantly. In 2013, 68 percent of clients were suppressed. By 2015, 80 percent of clients were suppressed. Congratulations to the 2016 NQC Award for Measurable Improvements in HIV Care.
Family First Health: Caring Together Program
Family First Health is a community health center with five sites serving approximately 28,000 clients in South Central Pennsylvania. The Caring Together Program has been receiving RWHAP Part B and C funding since 1991 and serves approximately 550 clients.
In July 2014, Caring Together embarked on a 2-year quality improvement project focused on retention. Using the in+care Campaign's definition of medical visit frequency, in August 2014, data indicated a retention rate of 64 percent. Over a 2-year period, the program had seen a drop in medical visit frequency of 8.6 percent. The clinical quality management committee focused on using data to explore disparities and identify barriers to care. Several issues were found, including a glitch in CAREWare, process problems, and a disparity in the data for clients falling under 100 percent of poverty. After the CAREWare issue was resolved, the rate increased to 70 percent.
In response to the findings, processes were revised. The processes for refilling medications and completing lab work were streamlined and the process for reviewing out-of-care clients was improved. The CDC's Anti-Retroviral Treatment and Access to Services (ARTAS) intervention was also implemented. ARTAS is an individual-level, multi-session, time-limited intervention with the goal of linking recently diagnosed persons with HIV to medical care soon after receiving their positive test result.
As of January 2016, medical frequency measure is at 77 percent-an increase of over 12 percent from baseline data. Over the study period, viral load suppression rates also increased from 84 percent to 88 percent. Congratulations to the 2016 NQC Award for Measurable Improvements in HIV Care.